All published articles of this journal are available on ScienceDirect.
Impact of Advances in Invasive Cardiology on Cardiac Surgery
Abstract
Background:
There is a noticeable decline in the number of patients who undergo coronary artery revascularization procedures. The change is definite as it is reported by many centers around the world. This trend is of great concern to cardiac surgeons because of its impact on their practice, its adverse effect on training and the degree of uncertainty it throws into future of the specialty.
Methods:
The data of the cardiac catheterization laboratory at the King Fahad Cardiac Center in the period between 1986 and 2006 was examined looking at the changing pattern of management of patients who undergo cardiac catheterization.
Results:
In the early years, angioplasty was attempted in around 10% of patients leaving the rest for surgical consideration or medical therapy. Currently only 15% of patients who undergo selective coronary angiography are referred for surgery. The majority are offered angioplasty and stenting. The trend is towards more catheter-based interventions and less towards surgery.
Conclusions:
Our findings are in agreement with the general consensus about the specialty. Cardiac surgeons should perhaps consider acquiring new skills which may be outside the operating room. Adding catheter based intervention particularly in valves to cardiac surgery training would be a bonus for the future surgeons that will give them the necessary edge to meet the new challenges. It is incumbent on the leaders in the field to establish a clear strategy for the future.
Mini-Abstract:
Impact of advances in invasive cardiology on cardiac surgery, based on actual analysis of the pattern of referrals to surgery of over two decades.
INTRODUCTION
It is a sign of the times; angioplasty and stenting are taking the lion’s share of coronary artery disease management. An important source for surgical material is diverted effectively reducing the surgical volume in many centers. The trend began with the introduction of percutaneous transluminal coronary angioplasty (PTCA).and slowly but surely took hold. It proved to be not a passing wave as it was initially thought of; on the contrary, it took hold and gave rise to a string of interventions each one leading to further reduction of the surgeons’ fortune. The range of modalities in interventional cardiology is ever increasing affecting other areas of the cardiovascular disease. It is taking advantage of new technology and successfully applying it to manage other areas in the spectrum of heart disease. We looked at the trend at our institution over a period of 20 years and noticed a definite reduction in the number of surgical referrals especially for coronary artery disease. If it is any comfort, we are in the same boat with the other centers who are witnessing a dwindling cardiac surgery volume. In order to study the dimensions of this change we looked at the factors that we believe are responsible for the shrinking volume. The root cause is not easy to pinpoint, but what is obvious is that while surgery remained stationary with a few cosmetic changes interventional catheterization underwent many revolutions. Cardiologists appear to be more open-minded in embracing new technology as it comes out adding to their armamentarium. Their unparalleled enthusiasm led to the great leaps in catheter-based interventions. The solution to the challenges facing cardiac surgery is not an easy one; it would take an integrated effort and to a degree has to come from within the surgical community. Surgeons should probably re think their role, and perhaps would need to be involved much earlier than they do now so that they can have a better say in the management of patients. In addition, they should perhaps be more receptive to new technology and implement it much more readily once it is considered safe.
MATERIAL AND METHODS
The cardiac catheterization laboratory (cath lab) data at the King Fahad Cardiac Center (The Center) for the period between August 1986 and December 2006 was examined. The aim was to analyze the pattern of disposition of patients following cardiac catheterization and any subsequent interventions. The total number of coronary angiograms performed over this period of time is 14814. All the patients who underwent cardiac catheterization were under the care of cardiologists who were responsible for the subsequent management decisions. Surgeons were consulted at the discretion of the cardiologists. Early on cardiologists insisted on having a surgical backup for every catheter-based intervention. This is now history as most of percutaneous coronary interventions (PCI) now are being performed without even informing the surgical team. They have a sense of security because they are certain that their colleagues the surgeons are always there ready and willing to help if and when needed.
Statistical Analysis
Data are expressed as mean ± standard deviation or median or range where appropriate. Analysis was performed by SPSS 11.5 (SPSS Inc. Chicago, Illinois). Significance was determined at p value of less than 0.05. All p values are two-sided and confidence intervals are 95%.
RESULTS
At The Center the change began slowly to take hold, the surgeons were obviously in a state of denial until it became evident that the downturn was permanent. In additon, most of the cases that are referred for surgery have a variety of co-morbid conditions adding to the surgical risk. Interestingly enough the problem is not unique to us as many other centers around the globe are experiencing a similar pattern [1, 2]. To validate this observation we examined the cardiac cath lab data for the period between August 1986 and December 2006. The current referral to surgery policy was compared to yesteryears referral practices. A total of 14814 coronary angiographies were carried out during this period of time. A significant number of the patients 40% had diabetes mellitus. The median hospital stay for cardiac catheterization was 4.3 days. The males constituted 65.5% of the group while the females were 34.5%. The mean age for the group as a whole was 56.7 while the mean age for males alone was 56.2 and for the females were 57.6. Left main disease was present in 1189 cases (8%), three vessel disease in 5037 cases 34%, two vessel disease 2815 (19%) and single vessel disease in 2783 (18%). In 2962 patients (20%) the coronaries were found to be normal in spite of the convincing symptoms the patients had, leaving a total of 11852 patients’ data to analyze, Fig. (1). Of the remaining 11852 patients, a total of 7704 (65%) cases were primarily managed by angioplasty stenting. The rest 4148 patients (35%) underwent primarily CABG 73.7 % of them had multivessel disease involving the LAD; the rest had either a double vessel disease including the LAD or a significant LAD lesion alone that was felt to be significant. Median hospital stay for the surgery group was 13.2 days.
In the angioplasty treated group acute coronary occlusion was encountered in 39 patients over the period of the study an incidence of 0.5% and was handled surgically in the early years; lately however, these complications are managed by deploying a bare metal or even a drug eluting stent leaving very little for surgery.
In the follow up of these patients, there was a 14.8% incidence of non-fatal myocardial infarction in the angioplasty treated group in the five years period that followed the intervention. In surgery, treated group 361 patients (8.7%) experienced the same in a five years follow up (p < 0.00001). Repeat catheterization was carried out because of recurrent stenosis causing symptoms in 27.4% of the angioplasty group and only in 7% of the patients who primarily had CABG, (p < 0.00001). During the of follow up period Coronary artery bypass grafting was eventually carried out on 19% of angioplasty stenting group because of recurrent stenosis not amenable to further interventions. The left main coronary hitherto untouchable by cardiologists is now being invaded in different clinical trials. At The Center, all left main disease is referred to surgery as the option of choice by the cardiologists. PCI for the left main was however carried out lately on five patients who posed unacceptable surgical risk. A drug eluting stent was successfully deployed in four of them. One of these patients succumbed during the intervention. The short-term follow up is uneventful. The success in these cases encouraged some cardiologists to recommend PCI for left main lesions that looked suitable for stenting citing the trials of other clinical centers in spite of the fact that stenting it with a DES is an off label use. [3, 4] .The evidence is compelling that CABG should indeed remain the preferred revascularization treatment in good surgical candidates with unprotected left main stenosis because of its substantial survival advantage and freedom from repeat intervention. PCI may be a reasonable option in those with isolated left main stenosis not involving the bifurcation or those in whom CABG is deemed too risky. However, PCI (with or without stents of any type) has not been shown to confer any survival advantage compared with medical therapy in any category of patients with stable coronary artery disease, and concerns remain over the risk of stent thrombosis with DES [5, 6].
DISCUSSION
Procedures involving stent deployment are referred to as percutaneous coronary interventions (PCI) to distinguish them from the plain angioplasty; percutaneous transluminal coronary angioplasty (PTCA). Patients undergoing a percutaneous coronary intervention outnumber those with coronary artery bypass surgery by a factor of 2 to 4. The default approach to PCI is the implantation of a drug-eluting stent (DES), in spite of the fact that it improves the results of balloon angioplasty only in about 25% of cases [7, 8] It is interesting to note that Andreas Gruentzig who is considered the father of interventional cardiology started the first technical revolution in 1977 when He introduced balloon percutaneous transluminal coronary angioplasty (PTCA) and envisioned that only around 10 to 15% of patients with coronary artery disease were treatable by angioplasty [9]. The irony is that these figures represent the number of cases that are currently referred to surgery Fig. (2). The second revolution is probably the introduction in the mid 80’s of intra-coronary stents deployed at the site of the atheromatous lesion. The recent addition is the drug eluting stents (DES) also referred to as "coated stents" that were received with great enthusiasm leading to much publicity because of its off label use in about 60% of the time and is lately embroiled in serious controversy [10, 11]. As expected in order to make up for the shortcomings of the DES a fully bioabsorbable one is now being used. The short-term results have shown that the in-stent late loss was 0.44 mm at six months and the restenosis rate was 11.5% [12, 13].
In view of the benefit, others and we have shown for coronary-artery bypass grafting, the real issue is why patients with symptoms and anatomy known to benefit from the procedure are still offered percutaneous coronary intervention [14]. Another point of equal interest is that patients with left ventricular ejection fraction >/=40% with a history of PCI prior to surgery had a worse outcome post CABG than those with no prior PCI. This is an important point to remember even though it is not certain if these results apply to drug eluting stents [15].
PCI has its place, but it should be offered to a selected group of patients. As an initial management strategy in patients with stable coronary artery disease, PCI does not reduce the risk of death, myocardial infarction, or other major cardiovascular events when added to optimal medical therapy [16].
A considerable number of our patients are diabetics; the available evidence clearly shows the superiority of surgery in this subset of patients. It has been shown that CABG is superior to PCI in this subset of patients. More recently, it has been demonstrated that type 2 diabetes mellitus is a major risk factor for in-stent restenosis. This is related to the increased serum malondialdehyde-modified low-density lipoprotein (MDA-LDL) concentration. Increased levels of MDA-LDL might be a consequence of metabolic abnormalities caused by diabetes. It is thought that it may act as a growth factor for neointimal tissues inside the implanted stent [17]. This is yet another reason that surgery should be the option of choice for diabetic patients.
Surgery reduces the number of re-interventions compared to PCI with drug-eluting stents, CABG results in improved major adverse cardiovascular and cerebrovascular event in patients with 2- and 3-vessel coronary artery disease, primarily in those with underlying diabetes [18, 19].
Our data showed improvement in the long-term survival for those who underwent surgery as the primary treatment option compared to those who underwent PCI as the primary therapeutic option but the difference is not as substantial as reported by others [20]. This is most probably due to the high incidence of diabetes mellitus in our patients.
Looking at other areas of cardiac surgery it is interesting to note that for a long time surgeons thought valves are their secure domain this was true until Zaibag [21] introduced percutaneous mitral valvotomy for mitral stenosis using double balloon. Many congenital heart diseases are now treated by the cardiologists (PDA, ASD, VSD, Coarctation, PS, distal pulmonary stenosis, and many others. Cardiologists have the patients and are armed with the latest catheter-based advances their literature reveals how far ahead they are. Valvuloplasty for calcific aortic stenosis, percutaneous implantation of the pulmonic valve and mitral valvuloplasty among others are slowly but surely becoming a routine like coronary stenting [22-24].
Percutaneous heart valve replacement and repair has emerged as an alternative to surgery. Thus one of the last remaining safe havens of surgery, treatment of valvular heart disease, is now being aggressively challenged by cardiologists. It seems that interventional Cardiology is now closer than ever to cardiac Surgery.
COMMENT
Realistically cardiac surgery did not reach this stage over night; it was years in the making. In order to deal with this impact on surgery there must be a clear strategy through recognized bodies of the specialty to tackle this challenge because of its implication on training of future cardiac surgeons. For years, surgeons have quibbled over on or off-pump grafting, tissue or mechanical valves but the fundamental operations are unchanged. In the mean time, other fields of medicine have rapidly advanced.
Another issue that is responsible for decreasing caseload is the ever-increasing number of centers that have open-heart surgery programs. Left unchecked the current environment is not very conducive for training future cardiac surgeons, as most of the cases because of their complexity are usually done by the staff surgeons leaving very little for the trainees. The problem is multifactorial one and the approach should be with that understanding.
- One of the major problems is that cardiac surgeons practice as end of the line referral-based specialists. The patient is evaluated by a series of physicians before is finally seen by the cardiac surgeon. It is becoming clear that surgeons should have their input early on so that the patient becomes well informed and can make an intelligent choice.
- Even though cardiac surgeons are also general thoracic surgeons by training but they have given up all of thoracic surgery and some have even in the care of their patients in the ICU for the intensivist. In the heydays of cardiac surgery during the 70 cardiac surgeons gave away pacemakers.. In the 80s, Automatic Implantable Cardioverter Defibrillator (AICD) had the same fate.. A more rational approach is called for before making such decisions, as it is not an easy task regaining lost territories.
- It is time to refine those minimally invasive methods and try to apply them to as many procedures as possible. Robotic surgery should be encouraged and new applications for it are sought.. Given the choice of 2-5 year 80% success rate of a stent with antiplatelet treatment, versus a more than 90%, 15-20 year patency rate of LIMA-LAD without any drugs in a low risk patient, most cardiologist, and patients would opt for the stent.
Surgeons should come up with a truly minimally invasive CABG, like a totally endoscopic multi-vessel revascularization, the patient is home in a couple of days and back to work in a week. To be realistic until that can be achieved more and more patients will opt for non-surgical treatment. Another approach is perhaps the hybrid myocardial revascularization. It is based on the assumption that drug eluting stents (DES) are as good as vein grafts for type A or B coronary artery lesions; but not as good as LIMA to the LAD which has 97% patency at10 years, it is the only graft that has shown survival benefits. Hybrid procedures are an attractive option for high-risk patients like the obese and those with COPD or for patients who seek a less traumatic revascularization option. Hybrid coronary revascularization is a combination of minimally invasive coronary artery bypass grafting and percutaneous coronary intervention in patients with multivessel coronary artery disease. The concept is now 10 years old. Implementation was slow, but major developments have taken place. The surgical part of the procedure can be performed in a totally endoscopic fashion. Intraoperative graft angiography during coronary artery bypass grafting (CABG) procedures is one important benefit. The sequence of revascularization is not a settled issue yet. The surgeon can first complete the LIMA to LAD thus giving the cardiologist a protected heart and then the cardiologist can subsequently proceed with the PCIs [23, 24]. - Cardiac surgeons should be in the forefront of the evolving percutaneous valve procedures. The time to get involved is now while the technique is still in its infancy. They understand valve repair and can therefore contribute to the development of these procedures. Percutaneous valve procedures require the expertise of different specialists (cardiac surgeon, interventional cardiologist, echocardiographist and anesthesiologist) working as a team. New horizons for cardiac surgeons are opening up [25]. The industry is aware that success of this technology will depend on cooperation among the different specialists so they will spare no effort.
- The evidence about the superiority of surgical treatment of coronary artery disease compared to stenting angioplasty should be effectively used to spread the message to the primary care physicians and even cardiologists. This was proven after ten randomized trials have compared percutaneous coronary intervention and coronary artery bypass grafting in patients with multivessel ischemic heart disease. Survival was rather similar with both interventions but surgery greatly reduced the need for further intervention (from 20% with PCI to 5% with coronary artery bypass grafting [26].
One important fact remains and that is Cardiology itself is going through changes as the continued development of non-catheter based coronary imaging has the potential to radically alter the current cardiologist-cardiac surgeon relationship and makes surgical involvement in the patient care team essential [27, 28] .
CONCLUSIONS
Cardiac surgery is facing major new challenges, but with the rapid advances in technology, there is great potential for innovation. As less invasive surgery gains popularity and surgeons change their role from being end of the line referral-based specialists to active participant the pre-operative decision-making, the field is poised for a renaissance and this could indeed prove to be to be an exciting time for heart surgery. This might sound too unreal for some; but if I could only stir a controversy, I would feel that I have accomplished my mission in initiating the much-needed debate.

The results of 14814 coronary angiograms.
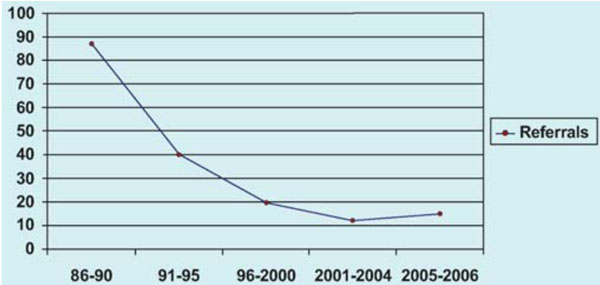
The changing pattern of referrals to surgery 1986-2006.


