All published articles of this journal are available on ScienceDirect.
The Relationship between the Risks of Developing Type 2 Diabetes Mellitus and Cardiovascular Diseases
Abstract
Background:
Type 2 Diabetes Mellitus (T2DM) has significantly increased in the past decades due to changes in lifestyles. This chronic disease is expected to be ranked in the seventh position by the year 2030 among the 15 leading causes of death. Poorly treated T2DM can be an important risk factor for cardiovascular diseases as well (CVD).
Objective:
We have sought to determine a relationship between the risks of developing T2DM and CVD in a healthcare facility in the district of Breña (Lima, Peru).
Methods:
The Finnish Diabetes Risk Score survey and the Pan American Health Organization risk calculator were used on a sample of 150 patients. The inclusion criteria were: patient age 40-80 years, attended their medical appointment more than once, were overweight or showed cholesterol levels above normal values and lived within the catchment area of the healthcare center where the study was carried out.
Results:
Only 8.7% of our sample was at a low risk of developing T2DM, whereas the rest was at a slightly elevated, moderate and high risk. Additionally, 79.3% of the patients were at low risk of developing CVD. Using the Fisher’s Exact test, there was a significant difference (p=0.026) between the risk of developing T2DM and CVD.
Conclusion:
The risk of developing CVD in our population is expected to rise in the future due to the high risk of developing T2DM. It is hoped that this work serves Peruvian (and other) health authorities to bolster their prevention programs, especially focusing on lifestyle interventions (e.g. increased physical activity), which have proven to be successful and economical.
1. INTRODUCTION
In the past decades, changes in lifestyles globally have brought about the propagation of some chronic diseases like Type 2 Diabetes Mellitus (T2DM), which in the past mainly affected adults but nowadays is also increasingly seen in children [1, 2]. Some of the risk factors for developing T2DM are overweight, age, family history of T2DM and a sedentary lifestyle [3].
Several studies have demonstrated that people of low socioeconomic status and with T2DM are more likely to suffer higher mortality rates [4-7]. Moreover, T2DM is more widespread in developing countries, because their health infrastructures do not have enough resources to prevent this kind of chronic disease [7]. Moreover, a study has indicated that diabetes mellitus, which was ranked in the 11th position in 2002 among the 15 leading causes of death, will be ranked in the 7th position by the year 2030 [8]. In 2017, the International Diabetes Federation (IDF) indicated that this disease affected 425 million people globally and it is predicted that by the year 2045, it will affect 629 million people [9].
Cardiovascular (CV) diseases (CVD) are the number one cause of deaths among people with T2DM [10]. Badly handled, T2DM can lead to CV complications and, in many cases, to high mortality rates [11]. People with T2DM are at 2-4 times higher risk of CV events than those who do not have T2DM [12].
The National Institute of Health (in Spanish: Instituto Nacional de Salud; INS), in Peru, has defined 11 public health crises to be of high priority for research between the years 2016-2021 [13]. Among these is diabetes mellitus. In the capital of Peru, Lima, it has been reported that the prevalence of diabetes has significantly increased from 4.4% in 2004 to 8.4% in 2011 [14]. Furthermore, a recent study has indicated that Peru has become one of the countries with highest incidence of diabetes worldwide [15].
The present study attempts to assess the relationship between the risks of developing T2DM and CVD in a population of patients from a healthcare facility in the district of Breña, in the Peruvian capital (Lima).
2. MATERIALS AND METHODS
A cross-sectional survey was carried out daily, during April 2019, to find out if there was a relationship between the risks of developing T2DM and CVD. The participants received help from the nurses working in a healthcare center located in Breña to complete questionnaires. It took each participant about 10-15 min to complete the survey.
The surveyed population included 150 men and women who attend a healthcare facility located in the district of Breña. The patients who visited this center suffered from different medical conditions (e.g. upper respiratory infections, fever, headaches) related to primary care. Only individuals who reported the following criteria were considered for the survey: age 40-80 years, attended a medical appointment more than once, were overweight or showed cholesterol levels above normal values and lived within the catchment area of the healthcare center where the study was carried out.
| Questions | |
|---|---|
| 1 | Age |
| 2 | Body-mass index |
| 3 | Waist circumference below the ribs |
| 4 | Do you usually have daily at least 30 minutes of physical activity at work and/or during leisure time? |
| 5 | How often do you eat vegetables, fruit or berries? |
| 6 | Have you ever taken medication for high blood pressure on regular basis? |
| 7 | Have you ever been found to have high blood glucose? |
| 8 | Have any of the members of your immediate family or others relatives been diagnosed with diabetes? |
The screening tool used to evaluate the risk of T2DM was the Finnish Diabetes Risk Score (FINDRISC) [16]. The questionnaire is made based on 8 questions (Table 1), which served to assess the risk of developing T2DM. FINDRISC categorizes the risk of developing T2DM, according to the total score of the 8 questions as: low, slightly elevated, moderate and high.
We measured the risk of developing CVD within the next 10 years, by using the Pan American Health Organization (PAHO) risk calculator (https://www.paho.org/ cardioapp/ web/#). In this questionnaire, six variables were considered: gender, age, smoking habit, systolic blood pressure, diabetes and cholesterol. The risk of developing CVD was categorized as: low, moderate, high and very high.
An association between the risks of developing T2DM and CVD was performed using IBM SPSS Statistics version 24.0 software. The Fisher’s Exact test for independence, was used for this purpose.
3. RESULTS
The ages of the 150 participants were between 40 to 78 years with a mean of 52.9 years (standard deviation 8.4). Table 2 shows the other characteristics of the participants.
| Number of participants | Percentage (%) | |
|---|---|---|
| Sex | ||
| Male | 88 | 58.7 |
| Female | 62 | 41.3 |
| Educational level | ||
| Primary | 26 | 17.3 |
| Secondary | 79 | 52.7 |
| Technical | 13 | 8.7 |
| Professional | 32 | 21.3 |
| Civil status | ||
| Single | 10 | 6.7 |
| Married | 63 | 42 |
| Divorced | 11 | 7.3 |
| Living together with a partner | 60 | 40 |
| Widow/widower | 6 | 4 |
| Occupation | ||
| Regular worker | 68 | 45.3 |
| Occasional worker | 59 | 39.3 |
| Unemployed | 10 | 6.7 |
| Retired | 12 | 8 |
| Housewife | 1 | 0.7 |
Some of the compelling results from the FINDRISC survey (Table 1) showed that 47 (31.3%) participants did not practice any physical activity on a daily basis. With regard to eating vegetables and fruits daily, 61 (40.7%) patients revealed that they did not eat these so frequently. Our results also showed that only 22 (14.7%) participants took medications for high blood pressure on a regular basis. Regarding high blood glucose levels; only 4 (2.7%) participants showed very high levels. For the question about history of diabetes in the family, 94 (62.6%) participants responded that there was no diagnosis of diabetes among their family members; 56 participants (37.3%) stated that parents, grandparents, uncles, aunts, or cousins had diabetes.
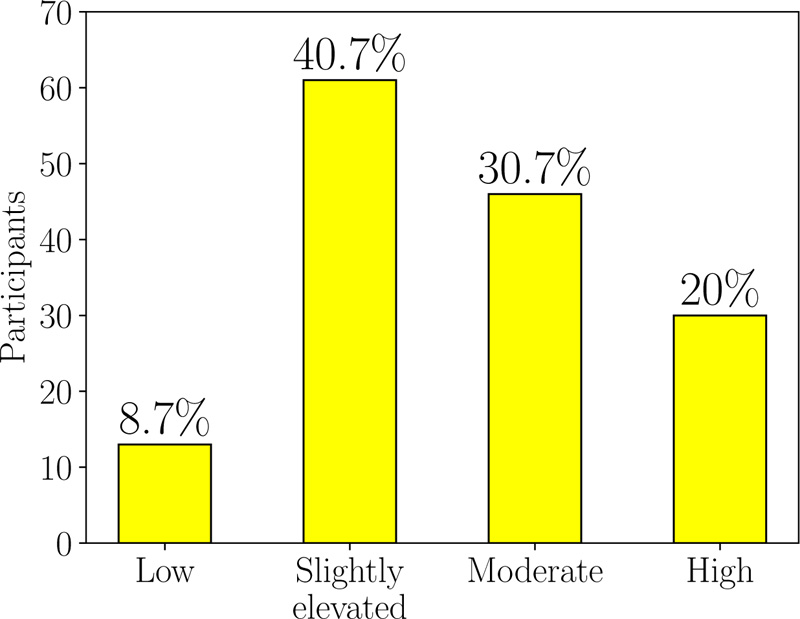
The FINDRISC classification of our surveyed population regarding the risk of developing T2DM is shown in (Fig. 1). It can be seen that 61 (40.7%) patients were at slightly elevated risk of developing T2DM. These were followed by 46 (30.7%) patients who showed a moderate risk. From the rest, 30 (20%) patients were at high risk of developing T2DM, whereas only 13 (8.7%) patients were at low risk.
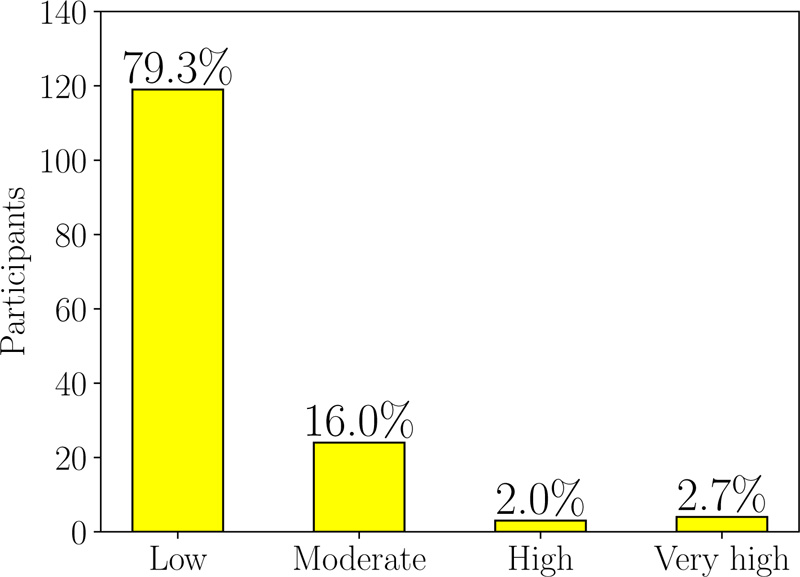
Regarding the risk of developing CVD (Fig. 2), 119 (79.3%) patients were at a low risk; 24 (16%), 3 (2%) and 4 (2.7%) patients showed moderate, high and very high risk, respectively.
We compared the risks of developing T2DM and CVD using the Fisher’s Exact test, which accounts for low frequencies in more than 20% of the cells (Table 3). There was a significant difference (p=0.026) between the risk of developing T2DM and CVD.
| T2DM | p | |||||
|---|---|---|---|---|---|---|
| Low | Slightly elevated | Moderate | High | |||
| CVD | Low | 12 | 51 | 37 | 19 | 0.026 |
| Moderate | 1 | 8 | 4 | 11 | ||
| High | 0 | 0 | 3 | 0 | ||
| Very high | 0 | 2 | 2 | 0 | ||
4. DISCUSSION
As indicated by a study [17], individuals with detrimental changes in their lifestyles, such as poor physical activity or increased smoking habit, can be at a greater risk of developing CVD. Likewise, a deleterious change in physical activity and other risk factors, indicated in Table 1, can increase the risk of developing T2DM in the next 10 years, as suggested by the results of this study [18]. Hence, due to the high risk of developing T2DM in our population, it is expected that in future, the CVD risk of this very same population will rise; this is because there is a tendency for weight gain and insulin deficiency with aging [19]. This suggestion goes in agreement with the fact that T2DM is a risk factor for CVD [20].
In order to decrease the probability that individuals at high risk will develop T2DM, prevention programs can be established during the prediabetes stage [21]; these programs will also help in preventing CV. Some successful programs involve lifestyle intervention and the administration of metformin and acarbose [22-24], both are antidiabetic drugs. Among the aforementioned measures, lifestyle intervention has proven to be the most beneficial for patients with risk of developing T2DM. This can be implemented through campaigns that set the weight loss goals, increase physical activity and promote the reduction of the intake of total and saturated fats [24]. Such enterprises, not only in Breña, but in different districts of the Peruvian capital can be organized with the support of the Peruvian Ministry of Health and other health institutions. This advice could also be applied to other nations worldwide.
CONCLUSION
We surveyed 150 patients that attended a healthcare center located in the district of Breña. Only 8.7% of our sample patient's group was at a low risk of developing T2DM, whereas the rest were found to be at a slightly elevated, moderate and high risk of developing this chronic disease. Due to this high risk of developing T2DM by the majority of the participants, we expect than in the years to come, the risk of developing CVD in this population (currently at a low CVD risk) will increase substantially. We expect that this study will encourage the Peruvian Ministry of Health, health institutions and health practitioners in general to further promote intervention programs to prevent the risk of developing T2DM. A very successful and economical strategy in individuals at risk of developing T2DM can be the promotion of changes in lifestyle.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethics Committee of the Universidad de Ciencias y Humanidades, Lima, Peru.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Informed consent has been obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in GitHub at https://github.com/coto20/T2DM_CVD_BRENA
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this article.
ACKNOWLEDGEMENTS
We are very grateful to the nurses from the healthcare facility of Breña for their invaluable help in carrying out the surveys and also to the patients for completing the questionnaires.


