All published articles of this journal are available on ScienceDirect.
Acute Coronary Syndrome in the Young: Clinical Characteristics, Risk Factors and Prognosis
Abstract
Background:
To describe the characteristics of patients ≤40 years of age hospitalized for acute coronary syndrome, analyze the risk factors and identify the variables associated with prognosis.
Methods:
Case series of patients admitted between 2003 and 2012 inclusive in a tertiary hospital (123 consecutive cases admitted between 2003 and 2012), and case-control study (369 controls selected from the general population matched for sex and age with cases, at a ratio of 3:1). Outcome variables: Mortality, likelihood of survival without readmission for heart-related problems, extent of coronary disease as determined by coronary angiography and cardiovascular risk factors.
Results:
Mean age was 35.4±4.8 years and 83.7% of the participants were men. Myocardial infarction with abnormal Q wave (48%) and single-vessel involvement (44.7%) predominated. Intrahospital mortality was 1.6%. For the 108 patients eventually included in the follow-up, likelihood of readmission-free survival after 60 months was 69.3±4.8%. In the case group 36% of the patients admitted to using cocaine. Compared to controls, the prevalence in patients was higher for smoking (74.8 vs 33.1%, p<0001), diabetes (14.6% vs 5.1%, p=0.001), low HDL-cholesterol (82.9 vs 34.1%, p<0.001) and obesity (30.0 vs 20.3%, p=0.029). Decreased left ventricular ejection fraction (odds ratio=2.2, p=0.033) and smoking (odds ratio=7.8, p=0.045) were associated with readmission for coronary syndrome.
Conclusion:
Acute coronary syndrome in people younger than 40 years is associated with diabetes and unhealthy lifestyle: smoking, sedentary behavior (low HDL-cholesterol), cocaine use and obesity. The readmission rate is high, and readmission is associated with smoking and decreased ejection fraction.
INTRODUCTION
Acute coronary syndrome (ACS) is one of the main causes of hospital admission in western countries [1]. In fact, cardiovascular disease, particularly acute myocardial infarction, is the leading cause of death in these countries [2,3] Although the characteristics and clinical course of this disease in older age groups have been reported in depth [4], and clinical practice guidelines contain a section devoted specifically to older patients [5], younger patients have rarely been studied. This may be because the incidence of ACS in younger people is much lower than in older people, although the incidence varies depending on the population, the age limits considered and social changes [6-9].
A recent study in Spain found that people younger than 45 years of age accounted for 6% of all hospital admissions among men and 2% among women, but that the rates of hospital readmission were significantly higher than in the population in which the first event occurred at later ages [10]. Patients who have ACS at an early age are at risk for many potential years of life lost, and their post-event survival translates as substantial costs in terms of health and social resources consumed [11]. In recent decades there have been important changes in the exposure to risk factors for ACS, e.g. the increased prevalence of sedentary lifestyles, obesity, metabolic syndrome and diabetes, and the decrease in smoking.[12,13] Knowledge about current cardiovascular risk factors (CVRF) that are related with the appearance of angina or myocardial infarction can help focus preventive efforts on the main determinants of the incidence of ACS in younger people.
The aim of this study was to determine the clinical and prognostic characteristics in patients younger than 40 years of age who are hospitalized for ACS, identify the CVRF associated with the incidence and prognosis of ACS, and compare the frequency of exposure to these risk factors with the frequency in the same-aged general population.
PATIENTS AND METHODS
The case series that formed the basis of this study comprised all patients admitted to Hospital Universitario Nuestra Señora de la Candelaria in Tenerife (Canary Islands, Spain) between 1 January 2003 and 31 March 2012 with a diagnosis of debut of ACS who were ≤40 years of age. Because the patients were relatively young, they were all treated with coronary catheterization. This study was approved by the Bioethics Committee of the Hospital. A case-control study was designed with this group of patients as the case group.
Controls were participants enrolled in the "CDC de Canarias" cohort study who had never been diagnosed with ACS, and they were matched for sex and age with cases at a ratio of 3 controls per 1 case. This cohort has been described previously [13]. Briefly, this cohort was randomly recruited from the general population of the Canary Islands between 2000 and 2005, with a participation rate of 70%. The acronym CDC stands for cardiovascular, diabetes and cancer. All participants enrolled (n=6729) were interviewed to record their health and lifestyle antecedents including physical activity, smoking, alcohol consumption and other aspects (available at http://www.cdcdecanarias.org). Each participant also underwent a physical examination to record anthropometric data and vital signs, and each also provided a sample of venous blood after fasting.
Patients who met at least two of the following criteria were considered to have had ACS: i) clinical features consistent with ACS, ii) dynamic changes in the ST segment, inverted T wave or appearance of a new Q wave, iii) elevated troponin I concentration above the upper limit of normality (0.6 ng/mL), and iv) a coronary lesion compatible with ACS on angiography. All patients with an alternative diagnosis, particularly pericarditis or acute myocarditis, were excluded.
Antecedents of hypertension, diabetes mellitus, dyslipidemia, smoking and use of other toxic substances, particularly cocaine, were recorded for all patients. Persons were considered a smoker if they stated smoking at least one cigarette per day, and were considered an ex-smoker if they stated they had quit smoking at least one year previously. A diagnosis of hypertension was recorded if blood pressure was ≥140/90 mmHg during the hospital stay r if the patient was using antihypertensive treatment. A diagnosis of diabetes was recorded if fasting serum glucose concentration was >125 mg/dL or if the patient was using antidiabetic treatment. Dyslipidemia was recorded if the patient was taking statins or if serum cholesterol concentration was >240 mg/dL. Hypertriglyceridemia was recorded if serum triglyceride concentration was >150 mg/dL, and low HDL-cholesterol was noted if the concentration of high density lipoprotein (HDL) cholesterol was<40mg/dL in men or<50 mg/dL in women. Overweight was defined as a body mass index (BMI) between 25 and 29 kg/m2, and obesity was defined as a BMI ≥30.
Coronary angiography was done during the hospital stay, and lesions that reduced the lumen area by 50% or more were considered angiographically significant. Left ventricular ejection fraction (LVEF) was estimated by echocardiography, and was classified according to systolic functioning as normal (LVEF ≥55%) or decreased (slight decrease: LVEF between 40 and 54%; moderate decrease: LVEF between 30 and 39%; severe decrease: LVEF<30%). Six months after hospital discharge, annual follow-up was started. Each patient was contacted by telephone to obtain information on mortality and the likelihood of readmission because of ACS. Total follow-up time ranged from 6 to 60 months.
STATISTICAL ANALYSIS
The results for scalar variables are expressed as the mean ± standard deviation or as the median and interquartile range for variables that did not follow a normal distribution. The results for categorical variables are summarized as absolute and relative frequencies (%).
To compare categorical variables we used chi-squared test or the Fisher exact test as appropriate, and calculated odds ratios (OR) with 95% confidence intervals (95% CI). For continuous variables we used Student’s t test or the Mann-Whitney test when the results were not distributed normally. For paired data (comparisons between cases and controls), we used the MacNemar test for binary outcomes and the paired t test student for continuous variables. Only bilateral hypotheses were considered, and a p value <0.05 was considered statistically significant.
The probability of survival was estimated with the Kaplan-Meier method. Cox multivariate regression models, stratified on the matching pairs, were used to estimate adjusted relative risk (RR) of hospital readmission for the three variables (smoking, diabetes and decreased LVEF) that showed an association with this risk at p<0.10 in the bivariate analysis; the dependent variable in these models was time to readmission for ACS or the end of follow-up. The assumption of proportional hazards was evaluated by analyzing the interaction of smoking with time to the event. All analyses were done with SPSS software (v. 19 in Spanish).
RESULTS
During the study period 123 young patients were admitted to our hospital with a diagnosis of ACS. Their mean age was 35.4±4.8 years, and 83.7% were men. There were no differences in age at first presentation between men and women (35.3±4.8 and 35.5±4.7 years, respectively). The clinical characteristics of our patients during their hospital stay are shown in Table 1. A diagnosis of myocardial infarction with abnormal Q wave predominated (48.0%), as did involvement of the diaphragmatic surface (39.2%), when the involved area could be located. However, the coronary artery involved most frequently was the anterior descending artery. Involvement of a single vessel was more common than multiple vessels, and in one third of the cases (29.3%) angiography showed that the lesions did not occlude more than 50% of the lumen diameter. The only coronary artery anomalies identified that were unrelated with atherosclerosis were diffuse ectasia in 1 patient and a circumflex artery originating from the right coronary sinus in 1 other patient. There were no significant lesions in the left main trunk.
Clinical characteristics of patients in this series with acute coronary syndrome.
| Diagnosis STEMI 73 (59.3) Non-STEMI 29 (23.6) Unstable angina 21 (17.1) |
Number of vessels involved 1 55 (44.7) 2 25 (20.3) 3 7 (5.7) Lesions occluding <50% 36 (29.3) |
| Location of infarction Inferior 40 (39.2) Anterior 31 (30.4) Lateral 4 (3.9) Not locatable 27 (26.5) |
Location of the lesion Anterior descending 54 (43.9) Right coronary 40 (32.5) Circumflex 29 (23.6) |
| Left ventricular ejection fraction >54 80 (65.6) 40-54 35 (28.7) 30-39 6 (4.9) <30 1 (0.8) |
Revascularization Percutaneous Drug-eluting stent 40 (32.5) Non-drug-eluting stent 20 (16.3) Both stents 4 (3.3) Surgical 10 (8.1) |
| Hospital course Killip classification I 112 (91.1) II 5 (4.1) III 0 (0) IV 6 (4.9) |
VF/VT * 5 (4.1) Papillary muscle rupture1 (0.8) Hospital death 2 (1.6) |
* VF/VT = Ventricular fibrillation or tachycardia.
Comparison of cases with acute coronary syndrome (n=123) and age- and sex-matched controls from the general population (n=369).
| Cases N (%) | Controls N (%) | OR (95% CI) | p | |
|---|---|---|---|---|
| Smoking | 92 (74.8) | 122 (33.1) | 5.98 (3.77-9.49) | <0.001 |
| Hypertension | 32 (26.0) | 77 (20.9) | 1.630 (0.81-2.09) | 0.316 |
| Diabetes mellitus | 18 (14.6) | 19 (5.1) | 3.34 (1.68-6.66) | <0.001 |
| Obesity | 36 (30) | 75 (20.4) | 1.67 (1.05-2.67) | 0.526 |
| Prior dyslipidemia | 34 (27.6) | 67 (18.2) | 1.73 (1.08-2.79) | 0.022 |
| Hypertriglyceridemia | 48 (39.0) | 88 (23.8) | 2.04 (1.32-3.16) | 0.001 |
| Low HDL-cholesterol | 102 (82.9) | 126 (34.1) | 9.37 (5.59-15.70) | <0.001 |
| Mean ± SD | Mean ± SD | |||
| Total cholesterol (mg/dL) | 168.17 ± 49.68 | 197.07 ± 38.39 | NA | <0.001 |
| LDL cholesterol (mg/dL) | 97.99 ± 35.02 | 125.30 ± 33.91 | NA | <0.001 |
| HDL cholesterol (mg/dL) | 33.93 ± 9.44 | 46.83 ± 11.57 | NA | <0.001 |
| Triglycerides (mg/dL) | 165.49 ± 97.99 | 127.41 ± 105.55 | NA | <0.001 |
NA: Not applicable.
Differences between patients readmitted for coronary syndrome or patients who died (n=31) during follow-up and other patients (n=79).
| Readmitted or died N (%) | Not readmitted, alive at the end of follow-up N (%) | p | |
|---|---|---|---|
| Age: Mean (Q1-Q3) | 36 (17-40) | 37 (27-40) | 0.500 |
| Sex (male) | 25 (80.6) | 69 (87.3) | 0.379 |
| Hypertension | 8 (25.8) | 20 (25.3) | 0.958 |
| Diabetes mellitus | 0 (0) | 16 (20.1) | 0.005* |
| Smoking | 30 (96.6) | 62 (78.5) | 0.041* |
| Cocaine use | 12 (38.7) | 29 (36.7) | 0.845 |
| Dyslipidemia | 11 (35.5) | 20 (25.3) | 0.286 |
| Coronary occlusion >50%# | 22 (71) | 54 (68.4) | 0.790 |
| Involved vessel | |||
| Anterior descending | 13 (41.9) | 32 (40.5) | 0.891 |
| Circumflex | 10 (32.3) | 15 (19) | 0.135 |
| Right coronary | 8 (25.8) | 29 (36.7) | 0.276 |
| Percutaneous revascularization | 18 (58.1) | 12 (38.7) | 0.940 |
| Diagnosis | |||
| STEMI | 18 (58.1) | 45 (57.0) | |
| Non STEMI | 8 (25.8) | 19 (24.1) | |
| Unstable angina | 5 (16.1) | 15 (19.0) | 0.936 |
| Decreased LVEF** | 13 (41.9) | 20 (25.6) | 0.095 |
* With continuity correction. ** Left ventricular ejection fraction <55%. # Before revascularizaction.
In 52.1% of the patients revascularization was done percutaneously, and in 8.1% surgery for aorto-coronary bypass was done during the initial episode. Complications during the hospital stay included ventricular fibrillation or sustained ventricular tachycardia in 5 patients (4.1%) and cardiogenic shock in 6 (4.9%). Seven patients had moderate or severe left ventricular dysfunction; during their inpatient stay 2 patients died (1.6% of all patients admitted [One died for cardiogenic shock and for other ventricular fibrillation]). Cocaine use was reported by 44 patients (36%) and was much less frequent among those with diabetes (6% vs 41%, p=0.009); 19% of the patients reported having used cocaine during the week of their event.
The analysis of events (mortality and readmission) included only the 110 patients who were followed for at least 6 months after discharge. Two patients were lost to follow-up because they moved to a different location. So, patients eventually included in the follow-up were 108. During a mean follow-up period of 52 months (range 8-133), 29 patients were readmitted for ACS (26.4%) and 4 of them died (2 during their hospital stay [both died for myocardial infarction] and 2 who died outside the hospital [One died for sudden death, and one for heart failure]). The estimated probability of survival at 60 months was 95.8±2.4%, but survival free from readmission for heart problems was 69.3±4.8% during this period. Among patients who were readmitted, 14 had acute myocardial infarction (48.3%). Cardiac catheterization was required again for 23 patients (20.9%) after discharge, and 15 (13.6%) required other revascularization procedures.
Table 2 compares the prevalence of CVRF in patients and controls. The prevalence of smoking was more than twice as high among cases as among controls (74.8% vs 33.1%, p<0.001) and the prevalence of diabetes was almost threefold as high (14.6% vs 5.1%, p=0.001), mainly owing to the diagnosis of type 2 diabetes. The frequency of overweight in the case group (34%) did not differ significantly from the control group, but the prevalence of obesity was significantly higher in the former group (30.0% vs 20.3%, p=0.029). The higher frequency of hypertension in the case group tended toward significance (26% vs 21%, p=0.056). The prevalence of dyslipidemia and mean triglyceride concentration were significantly higher in the case group, and the mean HDL cholesterol concentration was lower. In the case group, 83% of the patients had low HDL-cholesterol versus 34% in the control group (p<0.001). However, serum total and low density lipoprotein (LDL) cholesterol concentrations during hospitalization were lower in the case group than the control group.
Table 3 compares patients who were readmitted for heart-related problems or who died during follow-up with all other patients. There were no differences in age, sex, location of the coronary lesion, diagnosis, presence of hypertension, dyslipidemia, the percentage of patients who underwent percutaneous revascularization. There were no significant differences in the rate of readmission or exitus among patients without obstructive coronary lesions (27%), those who had lesions in one vessel (27%) and those with 2 or more injured vessels (32%). However, the percentage of smokers was higher among patients who were readmitted (p=0.020), and the frequency of diabetes was lower (none of the readmitted patients had diabetes; p=0.005).
Multivariate analysis to estimate RR for death or readmission yielded an RR of 2.2 for decreased LVEF (95% CI=1.1-4.5, p=0.033) and 2.7 for smoking (95% CI=0.9-7.7, p=0.064). When smoking was stratified for current, ex-smoker or never smoker status the RR for current smokers was 7.8 (p=0.045), although the confidence interval was broad (95% CI=1.1-57.3) because only 1 of 18 never-smoker patients was admitted. Figs. (1 and 2) show the event-free survival curves according to smoking and LVEF impairment. Relative risk estimates for diabetes could not be calculated because no patients with diabetes were readmitted.
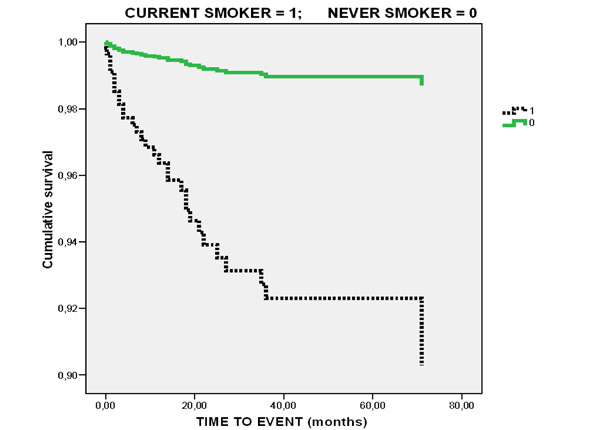
Survival curve for patients who were not readmitted and who did not die after an average follow-up of 60 months after the first event: Smokers vs. never smokers.
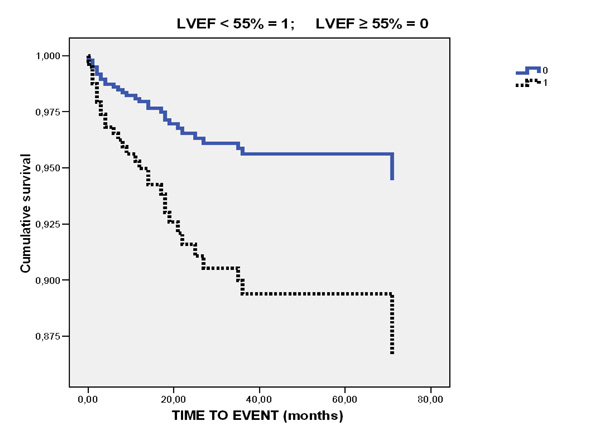
Survival curve for patients who were not readmitted and who did not die after an average follow-up of 60 months after the first event: Patients with and without decreased left ventricular ejection fraction after their first hospitalization for acute coronary syndrome.
DISCUSSION
Unlike most earlier series of young patients with ACS, our comparison of cases and controls drawn from the general population makes it possible to quantify the magnitude of risk factors in these patients. We show that compared to the general population of the same age and sex, patients aged 40 years or less diagnosed as having ACS had an unhealthy lifestyle: cocaine use was frequent and the prevalence of smoking, obesity, low HDL-cholesterol and diabetes was higher. Although mortality during their first hospital stay was low, the readmission rate was high and readmission was associated with smoking and decreased LVEF.
Given the young age of our patients with coronary syndrome, we supposed the proportion of patients with non-atherosclerotic lesions would be greater than that found. Anomalous origin of the circumflex artery was observed in only 1 patient, and this finding was unrelated to the clinical findings; 1 other patient had signs of possible vasculitis. The low frequency of coronary artery disease among our patients is also a feature in other series of young patients in whom the disease often involves only one or two vessels, and a large percentage of patients had no relevant coronary lesions. The percentage varies widely across studies, but is higher than 20% and can be as high as 30% [14-17], as in the present series, although not all studies reported angiographic findings systematically. The relatively low frequency of coronary artery disease may have a number of causes. Firstly, a small proportion of patients labeled as having myocardial infarction or unstable angina may have been misdiagnosed and therefore misclassified. Although they met the clinical, enzymatic and electrocardiographic criteria, alternative diagnoses such as myocarditis are a possibility; however, myocarditis is hard to distinguish from ACS without the use of techniques such as myocardial biopsy or magnetic resonance imaging [18], neither of which was used in our patients. Secondly, the main risk factor in young patients is smoking, and exposure in our case group was sixfold as high as in our control group from the general population. We had no data on persistence of smoking, so the relevant variable in our study was smoking at baseline. It was reported that lesions in smokers often contain large thrombi which may remain present in a plaque that occupies a small area of the lumen after antiaggregant, anticoagulant or fibrinolytic treatment [19]. A third explanation lies in the role of vasospasm induced by cocaine or smoking, although provocation tests are not usually used in our hemodynamic laboratory.
In addition to smoking, the patients in our series had other characteristics related with unhealthy lifestyle habits. Despite their relative youth, one third of the patients were obese – a significantly higher proportion than in the control group from the general population. This finding, as well as the high prevalence of low HDL-cholesterol, can be attributed to greater sedentary behavior. The prevalence of diabetes (mainly type 2 despite their age) was threefold as high in the case group as in the control group, a difference that may also be related to obesity and lack of physical activity.
Interestingly, diabetes was associated with the incidence of ACS in younger patients but not with readmission or death. There are several explanations for this apparent paradox: the time elapsed since diagnosis of diabetes is less clearly related with the macrovascular risk (ACS in the present study) than with the microvascular complications [20] Although the prognosis for acute myocardial infarction is known to be worse in patients with diabetes, these patients tend to be mature adults [10]. The pathophysiological substrate in the endothelium may be different in young patients, in whom prethrombotic status and instability of the incipient plaques are predominant features attributable to smoking, as opposed to the diffuse lesions that typify long-term diabetes. In this connection, the morphological pattern and angiographic distribution of the lesions in our group of patients were not those typical of diabetes. Moreover, the findings may have been influenced by interference from factors such as vasospasm caused by cocaine, which is used more frequently by young adults without diabetes.
A notable finding is that 36% of our patients reported using cocaine. Aside from the possibility of underreporting, this very high prevalence has been reported previously in young patients hospitalized for myocardial infarction or angina [21], and is a fact that should alert us to the role of this substance in the appearance of ACS in this age group. Although we had no information regarding substance use in our control group, cocaine use in our case group was much higher than the prevalence of exposure reported in the general population in Spain [22]. Our finding that cocaine use was associated with the incidence of ACS but not with the risk of readmission may be attributable to patients’ decision to stop using this substance after their first event, but this possibility awaits further research. We found cannabis users among cases, although this is an association that has also been described previously[23].
The higher frequency of previous dyslipidemia in our case group can also be related with lifestyle in these patients. Although serum total and LDL cholesterol concentrations appear to be contradictory, these values should be considered in the light of the fact that blood samples were obtained more than 48 h after admission. The concentration of LDL is known to decrease soon after ACS, whereas no such decrease occurs for HDL cholesterol or triglycerides [24].
The readmission-free survival curves were clearly worse for patients who were smokers. The negative effect of smoking on coronary events after myocardial infarction in young patients has been reported in earlier research [25]. This finding underscores the importance of intensive efforts to reduce toxic habits in these patients. The lack of association between lesions that occluded more than 50% of the vessel lumen and the risk of readmission suggests that the prognosis for young patients with ACS cannot be linked to their angiographic findings. In contrast, diminished LVEF and smoking are better markers of the likelihood of readmission. Although the prognosis is good during the hospital stay for the first episode, the high likelihood of readmission for heart-related problems during follow-up indicates that young patients with coronary artery disease are highly likely to consume considerable healthcare resources [11].
The main limitations of our study can be attributed to the small sample size; nevertheless, few series have assembled larger samples given the low incidence of ACS in young people. A strength of our study is that we compared cases with a control group drawn from the general population. Other limitations are the fact that the data for patients were obtained from medical records, which are always incomplete, and the lack of magnetic resonance imaging results, which would have provided important information. The high prevalence of cocaine use and the unexpected lack of events in diabetic may make our data not fully representative of the whole population of young patients with ACS, and data regarding substance use was available and analyzable only for patients, but not for individuals in the control group.
CONCLUSION
The incidence of ACS in our sample of young patients was associated with type 2 diabetes and unhealthy lifestyle that included cocaine use, smoking, obesity and low HDL-cholesterol. Although mortality was low during the first hospital stay, the readmission rate was high – a finding associated with smoking and decreased LVEF after the first myocardial infarction. The rapid spread of obesity and diabetes can be expected to increase ACS in young people in the coming years. Improving lifestyle is a goal of the first magnitude in these patients.
DISCLOSURES
None. We have not any kind of competing interest.
ABBREVIATIONS
| ACS | = Acute coronary syndrome. |
| LVEF | = Left ventricle ejection fraction |
| CVRF | = Cardiovascular risk Factors |
| OR | = Odds ratio |
| CI | = Confidence interval |
FUNDING
Canarian Health Service.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGMENTS
K. Shashok for translating the manuscript into English.


