All published articles of this journal are available on ScienceDirect.
New Insights into the Management of Hypertension and Cardiovascular Risk with Angiotensin Receptor Blockers: Observational Studies Help Us?
Abstract
Post-marketing observational studies are valuable for establishing the real-world effectiveness of treatment regimens in routine clinical practice as they typically monitor a diverse population of patients over many months. This article reviews recent observational studies of angiotensin receptor blockers (ARBs) for the management of hypertension: the 6-month eprosartan POWER study (n~29,400), the 3-month valsartan translational research programme (n~19,500), the 9-month irbesartan Treat to Target study (n=14,200), the 6-month irbesartan DO-IT survey (n~3300) and the 12-week candesartan CHILI survey programme (n=4600). Reduction in blood pressure with ARBs reported across these studies appears to be comparable for the different agents, although direct comparisons between studies cannot be made owing to different treatment durations and baseline patient demographics. Of these studies, the eprosartan POWER study, 2 of the 7 studies in the valsartan translational research programme, and the candesartan CHILI Triple T study measured total cardiovascular risk, as recommended in the 2013 European Society of Cardiology-European Society of Hypertension guidelines. The POWER study confirmed the value of the Systemic Coronary Risk Evaluation (SCORE) to accurately assess total cardiovascular risk.
With the advent of new healthcare practices, such as the use of electronic health records (EHRs), observational studies in larger patient populations will become possible. In the future, algorithms embedded in EHR systems could evolve as decision support tools to inform on patient care.
INTRODUCTION
There is a common perception within the scientific community that observational studies overestimate treatment effects and as such, the validity of studies is often widely disputed [1, 2]. However, with the advent of new healthcare practices, such as the use of electronic health records (EHRs), observational studies with novel statistics conducted in much larger study populations will be possible and will allow conclusions to be drawn from observed trends [3]. In this article, the role of observational studies in cardiovascular (CV) research will be discussed and a critical review of recent observational studies with angiotensin receptor blockers (ARBs) will be presented. The main focus of the search strategy was to select a range of different ARBs to be compared: MEDLINE was searched for recent observational studies of ARBs involving large patient populations using the search terms ‘angiotensin receptor blocker’, ‘observational study’ and ‘clinical practice’.
ROLE OF OBSERVATIONAL STUDIES IN CARDIOVASCULAR RESEARCH
Controlled clinical trials are often considered as the gold standard to evaluate the safety and efficacy of new treatments. However, there are limitations to their use. Forexample, while the strict eligibility criteria for clinical trials reduce the influence of patient variability on outcome measures, these patient populations do not reflect the general population and/or those who may be prescribed the treatment in clinical practice. Therefore, it is possible that some treatment effects may not be detected during a clinical trial setting. In CV research, clinical trials for antihypertensive therapies do not always report total CV risk. The importance of total CV risk has been reaffirmed in the new guidelines for the management of hypertension issued jointly by the European Society of Cardiology and the European Society of Hypertension (ESC/ESH) [4]. Guidelines should be used to advise the selection of patients requiring treatment and to select the intensity of antihypertensive treatment regimens [4]. Observational studies offer some advantages over clinical trials [5]. Specifically, the follow-up period is often much longer than that of a clinical trial, therefore observational studies are more likely to detect rare adverse events or those caused by long-term treatment. In addition, observational studies are often conducted in routine clinical practice where the diversity of patients is much wider than in a clinical trial. Treatment effects, for example those associated with comorbidities or concomitant medications not permitted in a clinical trial, may be identified during an observational study thereby providing invaluable information.
Approximately 90% of research papers published in clinical speciality journals describe results from observational studies [5]. Evaluation of 99 reports, across 5 different clinical areas, by Concato and colleagues demonstrated that well-designed observational studies do not overestimate the magnitude of treatment effects compared with randomised controlled trials in the same clinical field [2]. In addition, Golder and colleagues reported that observational studies and randomised controlled trials appear to result in similar risk estimates for adverse events, which suggests that systematic reviews of adverse events should not be limited to clinical trials alone [1].
Clinical trials and observational studies therefore play valuable but distinct roles in providing evidence on treatment effects and neither should be considered in isolation when evaluating the overall efficacy and safety of treatments. With the recent publication of guidelines for performing observational studies [6] and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [5], physicians are better supported to assess the value of observational research and to have confidence in their results.
REVIEW OF RECENT OBSERVATIONAL STUDIES OF ARBs
The study designs and objectives of selected recent observational studies evaluating ARBs are provided in (Table 1). The following section will summarise the study objectives, design and results for each study:
Comparison of recent observational studies of angiotensin receptor blockers.
| Name (references) | Agent | Study design | Objective/ Primary endpoint |
Key points |
|---|---|---|---|---|
| POWER [10, 11] | Eprosartan (eprosartan 600 mg/day monotherapy or in combination with HCTZ 12.5 mg/day) |
6-month open-label observational study in 16 countries worldwide (n>29,000) |
Absolute change in SBP over 6 months of treatment and its impact on total cardiovascular risk | Significant reduction in SBP was irrespective of patient sex, age, diabetic status or cardiovascular history |
| Valsartan Translational Research Programme [12] | Valsartan (various formulations: valsartan 80 mg or 160 mg monotherapy or in combination with HCTZ 12.5 mg or 25 mg, amlodipine 5 mg or amlodipine 10 mg) |
Seven observational studies over 90 days involving 19,533 patients | Assess SBP and DBP control after 90 days of treatment. Total cardiovascular risk assessed in two studies (BSCORE and EXCELLENT) | Combined data from all studies demonstrated significant reductions in SBP and DBP |
| Treat to Targetstudy [15] | Irbesartan (irbesartan 75, 150 or 300 mg as monotherapy or in combination with HCTZ 12.5 mg) | Prospective, two-armed, post-authorisation 9-month observational study conducted in Germany (n=14,200) | Change in SBP and DBP after 9 months of treatment and its impact on criteria for the metabolic syndrome | Irbesartan monotherapy and in combination with HCTZ significantly reduced both SBP and DBP. The number of patients with the metabolic syndrome was reduced at the end of the observation period |
| DO-IT survey [16] | Irbesartan (irbesartan 150 mg or 300 mg daily with or without HCTZ 12.5 mg daily) |
Prospective, observational, 6-month study in Germany (n=3259) |
Change in blood pressure and metabolic parameters after 6 months of treatment in patients with the metabolic syndrome | Treatment resulted in significant reductions in SBP and DBP and improved metabolic measures |
| CHILI Triple T survey programme [18] |
Candesartan cilexetil (candesartan cilexetil 16 mg + HCTZ 12.5 mg [fixed-dose combination] or candesartan cilexetil 32 mg [high-dose monotherapy]) | Prospective, non-interventional, uncontrolled, open-label, 12-week observational study in Germany (fixed-dose combination, n=3337; high-dose monotherapy, n=1263) | Change from baseline in blood pressure (SBP and DBP) and cardiovascular risk | Both fixed-dose combination therapy and high-dose monotherapy effectively reduced blood pressure in patients at increased risk of cardiovascular events |
DBP, diastolic blood pressure; HCTZ, hydrochlorothiazide; SBP, systolic blood pressure.
Key observational studies of angiotensin receptor blockers: measures of cardiovascular risk.
| Studies that reported changes in total cardiovascular risk: | Studies that reported changes in cardiovascular risk parameters: |
|---|---|
|
|
Eprosartan POWER Study
Objectives
The primary objective of the Physicians’ Observational Work on Patient Education According to their Vascular Risk (POWER) study was to evaluate the change in systolic blood pressure (SBP) following treatment with eprosartan-based antihypertensive therapy for 6 months in a large population from countries with differing levels of total CV risk. The secondary objective of the study was to assess the total CV risk.
Study Design
The POWER study was a 6-month open-label, post-marketing surveillance study. Details of the study design and methodology are described elsewhere [7]. In brief, patients with mild-to-moderate hypertension (mean sitting SBP >140 mmHg) treated with eprosartan were recruited by general physicians (GPs) or cardiologists from 16 countries within Europe, the Middle East, Asia, Africa and North America. Patients were either newly diagnosed with hypertension or were unresponsive to or intolerant of their current antihypertensive treatment. Initial treatment was with eprosartan monotherapy (600 mg/day). If patients had inadequate blood pressure (BP) control after 1 month of treatment with eprosartan monotherapy, other antihypertensive agents (preferably hydrochlorothiazide [HCTZ] 12.5 mg/day) could be prescribed. Physicians retained the discretion to use other interventions such as lipid-modifying agents and smoking cessation initiatives.
Response to eprosartan-based therapy was defined as achievement of SBP<140 mmHg and/or a reduction in SBP ≥15 mmHg or diastolic blood pressure (DBP)<90 mmHg and/or reduction in DBP ≥10 mmHg. The change in CV risk after 6 months of treatment was calculated using either the Systemic Coronary Risk Evaluation (SCORE) [8] method or the Framingham score [9] (Canadian cohort only).
Results
Of the 29,370 patients included in the safety population, 26,192 patients were eligible for the intention-to-treat (ITT) cohort [10]. The mean age of the ITT population was 61.3 years and 52% of patients were male. Men had a significantly lower mean age compared with women (59.5 vs 63.3 years; p<0.01). There was also a difference in age distribution between the sexes, with women representing proportionally more (59%) of the older (>70 years) age group and men representing proportionally more (63%) of the 50-59 years age group.
Mean baseline arterial BP was 160.4 ± 14.3/93.6 ± 9.7 mmHg and mean pulse pressure was 66.9 ± 14.3 mmHg. SBP increased with age whereas DBP decreased with age, hence pulse pressure increased with age. Systo-diastolic hypertension and isolated systolic hypertension were recorded in 73% and 25% of patients, respectively. CV-relevant pathologies included diabetes (23%), left ventricular hypertrophy (19%) and arteriosclerosis (19%). There was a family history of CV disease in 40% of patients and 25% of all patients were smokers [10].
Treatments Prescribed
Approximately one-third of patients were assigned each to eprosartan monotherapy, dual therapy or multiple therapies. The most commonly prescribed supplementary drugs were beta-blockers, calcium antagonists, HCTZ or other diuretics, and angiotensin-converting enzyme inhibitors. The use of combination therapy was more common in men, in older or diabetic patients, and in those with a significant history of CV disease.
Key Efficacy Results
Mean SBP in the ITT population decreased by 25.8 ± 14.4 mmHg after 6 months’ treatment (p<0.001 vs baseline) (Fig. 1A). Significant reductions in the mean DBP (12.6 ± 9.5 mmHg) and pulse pressure (13.2 ± 13.5 mmHg) were also observed at 6 months (both p<0.01 vs baseline) (Fig. 1A). Antihypertensive treatment efficacy was demonstrated in all patient subsets, including those with diabetes or other forms of high baseline CV risk [10].
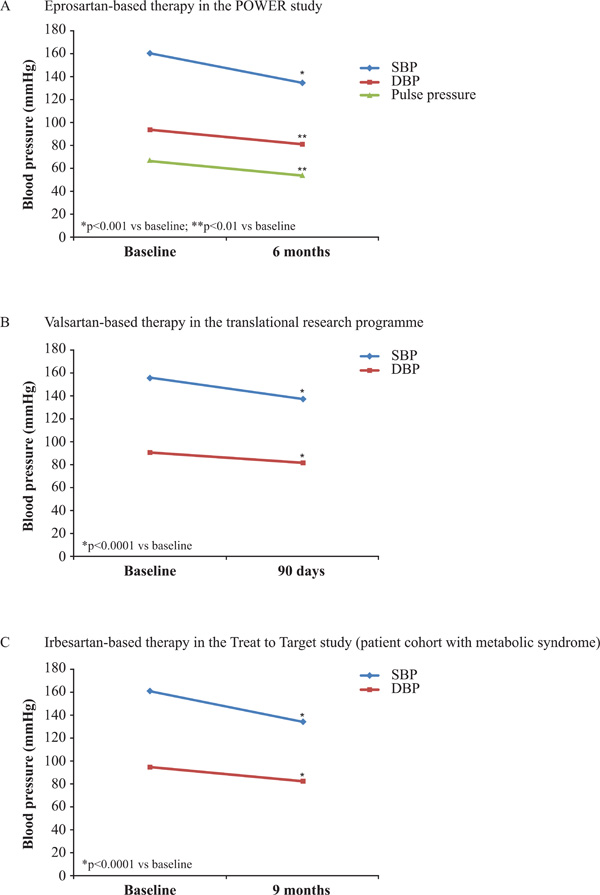
Reduction in blood pressure with angiotensin receptor blockers in observational studies [10, 12, 15]. DBP, diastolic blood pressure; SBP, systolic blood pressure.
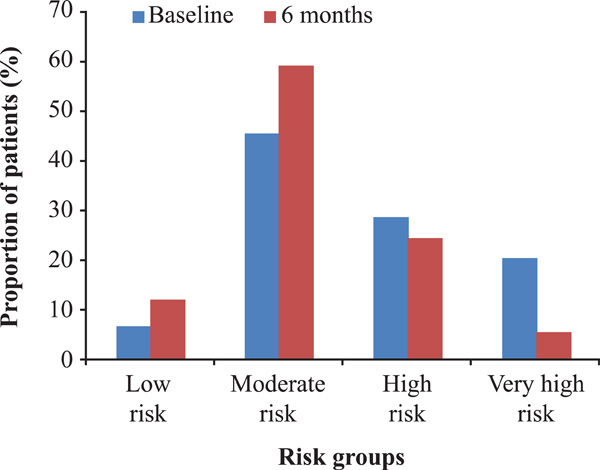
Chart-based estimates of SCORE risk distributions in the POWER survey at baseline and after 6 months of treatment with eprosartan-based therapy. Estimates are based on n=12,718 at baseline and n=9577 at 6 months. Low risk, <1%; moderate risk, 1–4%; high risk, 5–9%; very high risk, ≥10% [11].
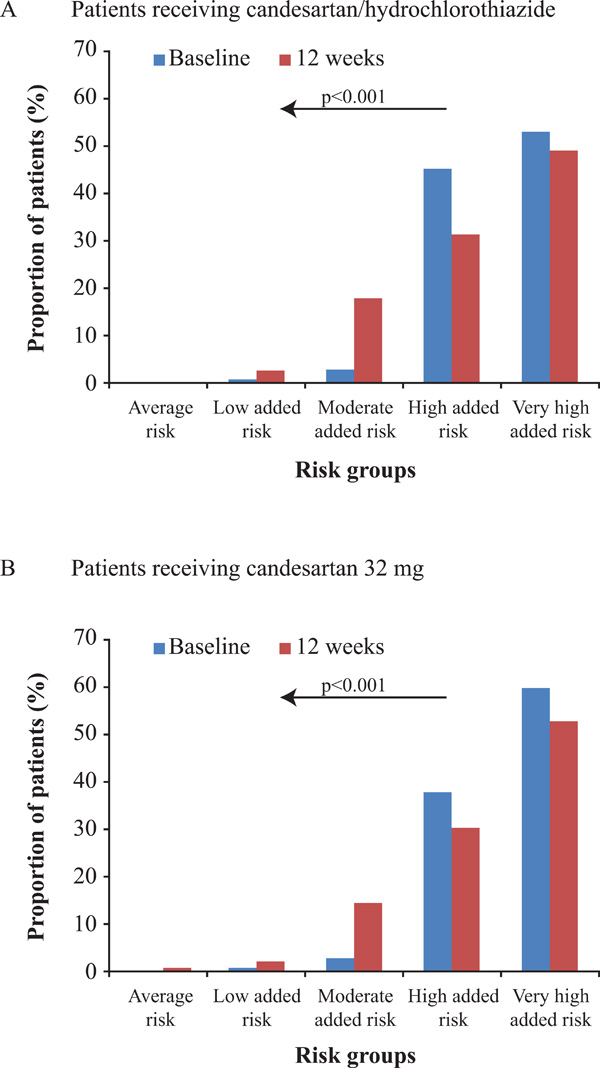
Cardiovascular risk (%) at baseline and after follow-up in the CHILI Triple T study [18] according to the European Society of Hypertension/European Society of Cardiology 2007 guidelines [19]. (A) Patients receiving candesartan/hydrochlorothiazide; (B) patients receiving candesartan 32 mg. Stratification of cardiovascular risk in four categories. Low, moderate, high and very high added risk refers to 10-year risk of a cardiovascular fatal or non-fatal event.
At the end of the observation period, approximately 62% of patients achieved the predefined target of SBP<140 mmHg and DBP<90 mmHg, and over 90% of patients were classified as ‘responders’ to eprosartan-based therapy.
The calculated total CV risk (SCORE or Framingham) reduced in parallel with the eprosartan-related reduction in SBP. In those patients for whom the SCORE risk estimation was applicable (n=12,718), the mean chart-based SCORE value was 6.0% ± 5.8% at baseline compared with 3.5% ± 3.5% after 6 months of treatment, corresponding to an absolute reduction of 2.4% ± 3.1% and a relative reduction in CV risk of 38.4% [11].
SCORE risk was stratified into 4 categories: low risk (<1%), moderate risk (1-4%), high risk (5-9%) and very high risk (≥10%). Analysis of the SCORE risk distribution at baseline and 6 months (Fig. 2) shows the change in distribution of CV risk distribution after 6 months of treatment. Three-quarters of patients initially classified as being at very high risk were reclassified to lower risk groups, of whom 11% were reclassified 2 categories below very high risk [11].
Safety
Eprosartan therapy, either alone or in combination with other antihypertensive treatments, was well tolerated. Adverse events were recorded in less than 2% of patients, two-thirds of which were recorded as suspected adverse drug reactions. Importantly, no new adverse drug reactions were identified in the safety population [10].
Valsartan Translational Research Programme
A translational research programme, comprising 7 observational studies on various valsartan regimens (monotherapy as well as single and separate pill combinations) was reviewed by Abraham and colleagues [12].
Objectives
The core objectives across the 7 studies were to assess SBP and DBP control at 90 days in patients receiving valsartan after failure of or intolerance to previous hypertensive treatment; to determine the percentage of variance in BP at 90 days attributable to a physician class effect; to examine the hierarchical determinants of BP at 90 days; and to identify independent predictors of non-response to valsartan-based treatment. In 2 of the studies (BSCORE and EXCELLENT) physician-reported total CV risk was assessed [13, 14].
Designs
All 7 studies were conducted in Belgium using the same methodological and statistical methods. The studies included a baseline assessment at initiation of valsartan treatment, and a follow-up assessment after approximately 90 days. The studies included only patient data collected as part of routine clinical practice.
Each study examined the impact of valsartan-based treatment regimens on SBP and DBP values and BP control, as defined by the 2007 ESC guidelines at the time the studies were conducted (SBP<140 mmHg and/or DBP<90 mmHg, except for patients with diabetes mellitus and/or a high or very high CV risk, in which case targets were 130/80 mmHg).
The 7 studies all included advanced modelling techniques to identify determinants of BP outcomes and CV risk, where relevant. Using a statistical hierarchical approach, in which patients were grouped under their treating physicians, the investigators examined both physician- and patient-related determinants of uncontrolled BP at 90 days and independent predictors of improved CV risk (BSCORE and EXCELLENT studies only).
Results
A total of 19,533 evaluable patients were contributed by 3434 physicians across the seven studies; the weighted average for age was 63.6 (±12) years, 50.3% of patients were male and 23.7% were diabetic.
SBP and DBP values at baseline and after 90 days of valsartan-based treatment were similar across the seven studies. Using weighted averages, SBP decreased from a mean (±SD) of 155.9 ± 15.4 mmHg to 137.5 ± 11.8 mmHg, while DBP decreased from 91.5 ± 9.6 mmHg to 82.0 ± 7.5 mmHg (Fig. 1B). Valsartan regimens were associated with absolute reductions in mean SBP of −18.4 mmHg (p<0.0001) and mean DBP of −9.5 mmHg (p<0.0001) compared with baseline values. At 90 days, 38.2% of patients had controlled SBP, 58.2% of patients had controlled DBP and 32.0% of patients had both controlled SBP and DBP.
Combined data from the BSCORE and EXCELLENT studies showed that the total CV risk classification decreased by 0.74 ± 0.95 of a category after 90 days of antihypertensive treatment. Over this period, the total CV risk was reduced by at least one category from baseline in 59.5% of patients. Improvements in total CV risk from baseline were statistically significant for both studies (p<0.0001).
The evidence from the translational programme was robust, with the findings being persistent across time, different formulations, patients and clinicians.
Irbesartan Treat to Target Study
Objectives
The main objectives of this study were to investigate the effect of irbesartan, either as a monotherapy or in combination with HCTZ on: BP response, metabolic parameters and resultant changes in CV risk factors [15].
Design
The study was a prospective, two-armed, post-authorisation 9-month study in patients with uncontrolled hypertension with the metabolic syndrome. Patients with uncontrolled hypertension but without the metabolic syndrome served as controls. It was conducted as an observational study in primary care by 3609 GPs in Germany. Patients were treated with once-daily irbesartan 75, 150 or 300 mg as monotherapy or in combination with HCTZ 12.5 mg, and additional antihypertensive medication was permitted. There were no specifications regarding BP targets, although many of the physicians followed the national guidelines.
SBP and DBP were measured at baseline and after 3 and 9 months of treatment. The following CV risk factors that make up the criteria for the metabolic syndrome were measured: changes in fasting glucose, waist circumference (a measure of abdominal obesity), serum triglycerides and high-density lipoprotein cholesterol (HDL-C). The proportion of patients fulfilling the criteria for the metabolic syndrome was also assessed.
Results
During the observation period (January 2005–July 2006), a total of 14,200 patients were documented, of whom 9281 had the metabolic syndrome and 4919 served as controls. The proportion of men and women and the mean age between the 2 groups were well balanced. Mean body mass index and waist circumference were higher in patients with the metabolic syndrome compared with the control group.
Overall, approximately 80% of all patients in the study received treatment with the highest dose of irbesartan (300 mg), either alone or in combination with HCTZ.
In patients with the metabolic syndrome, treatment with either irbesartan monotherapy or irbesartan in combination with HCTZ for 9 months resulted in significant reductions in BP. Irbesartan monotherapy reduced SBP and DBP by 26.3 ± 10.1 mmHg and 13.0 ± 6.6 mmHg, respectively (both p<0.0001) (Fig. 1C). Irbesartan in combination with 12.5 mg HCTZ reduced SBP and DBP by 27.5 ± 10.1 mmHg and 14.1 ± 6.6 mmHg, respectively (both p<0.0001).
Improvements in CV risk factors were observed with irbesartan monotherapy and were more pronounced in those patients with the metabolic syndrome. The addition of HCTZ to irbesartan in this cohort resulted in similar improvements in these parameters. Consequentially, there was a marked reduction in the number of patients fulfilling the criteria for the metabolic syndrome at the end of the observation period.
The overall tolerability throughout the study was very good with only 0.6% and 0.24% of patients reporting adverse events or serious adverse events, respectively.
These data are consistent with those reported for the DO-IT prospective, observational study, also conducted in Germany. In this study, the effect of 6 months of irbesartan treatment (150 or 300 mg daily) with or without HCTZ (12.5 mg daily) on BP and metabolic parameters was evaluated in patients with the metabolic syndrome (n=3259)[16]. Within the observation period, SBP decreased from 157.4 ± 14.7 mmHg to 135.0 ± 10.9 mmHg (−22.4 mmHg) and DBP decreased from 92.9 ± 9.2 mmHg to 80.8 ± 6.8 mmHg (−12.1 mmHg). The proportion of patients with SBP<130 mmHg increased from 1.6% at baseline to 20.4% after treatment, while the proportion of patients with SBP >180 mmHg decreased from 9.4% to 0.4%. Similarly, DBP was<85 mmHg in 15.7% of patients at baseline compared with 67% of patients at 6 months. The proportion of patients who had BP readings of<140/90 mmHg increased from 4.9% at baseline to 59.2% after 6 months of treatment. Improvements in metabolic parameters were also reported and were more pronounced in those patients who received the higher dose of irbesartan. An earlier observational study of 3 months’ irbesartan treatment in patients with hypertension and type 2 diabetes (n=16,600) reported a reduction in SBP/DBP together with a reduction in total CV risk, assessed using SCORE [17].
Candesartan CHILI Triple T Study
Objectives
The main objective of the CHILI (Candesartan in patients with Higher cardiovascular risk)Triple T study was to evaluate the efficacy and safety of candesartan cilexetil in a combination treatment regimen or as a high-dose monotherapy. The 2 treatment strategies were compared for achievement of BP targets in all patients, and for attaining BP targets in patient subgroups with different CV risks at baseline [18].
Design
The study was a prospective, non-interventional, uncontrolled, open-label, observational study conducted by GPs, internists or diabetologists in Germany. Patients with uncontrolled hypertension and added CV risk received a fixed-dose combination of candesartan cilexetil 16 mg and HCTZ 12.5 mg (combination therapy group) or candesartan cilexetil 32 mg (high-dose monotherapy group).
Results
A total of 4600 patients (3337 in the combination therapy group; 1263 in the high-dose monotherapy group) were included in the study (safety population) of which 4527 were eligible for efficacy analyses. Mean age was 63.1 ± 11.0 years and 55.3% of patients were male. Patients in the 2 treatment groups were comparable with respect to age and gender, but patients receiving high-dose monotherapy had a slightly higher mean SBP, more prior revascularisations, renal insufficiency, diabetic nephropathy, peripheral artery disease and a lower ankle brachial index.
Treatment with the combination therapy regimen reduced SBP by 28.5 ± 13.8 mmHg and DBP by 14.2 ± 9.4 mmHg (p<0.001 vs baseline values of SBP 160.2 ± 13.3 and DBP 94.5 ± 8.2 mmHg). High-dose monotherapy was also effective in reducing BP with reductions in SBP and DBP of 29.73 ± 15.3 and 14.1 ± 9.6 mmHg, respectively (p<0.001 vs baseline values of SBP 162.4 ± 14.7 and DBP 94.7 ± 8.7 mmHg).
Both the combination therapy and high-dose monotherapy groups had mostly high or very high added CV risk at baseline (see Fig. 3), as defined by BP readings and the presence of comorbid risk factors and disease according to the ESC/ESH 2007 guidelines [19]. CV risk was substantially reduced at the 12-week follow-up (p<0.001 vs baseline in both groups) with substantially fewer patients having high or very high added risk, and more patients having low or moderate added risk.
Overall tolerability throughout the study was very good with only 0.8% of patients in the combination therapy group and 1.2% in the high-dose monotherapy group experiencing an adverse event.
COMPARISON OF OBSERVATIONAL STUDIES
Post-marketing observational studies are valuable for establishing the real-world effectiveness of treatment regimens as they typically monitor a diverse population of patients over many months or even years. ARBs are routinely prescribed by both cardiologists and GPs, and regular monitoring occurs in routine clinical practice.
The 2013 guidelines from the ESC/ESH recommend that total CV risk is assessed systematically in all patients with arterial hypertension, for example by using the SCORE model. In addition, they recommend that the intensity of antihypertensive management is graded as a function of this risk [4]. Some, but not all, of the recent observational studies of ARBs presented in this review have reported measures of total CV risk (see Table 2). The relevance of those studies without total CV risk analyses, in terms of providing real-world insight, could be questioned since this measure is pivotal to inform treatment decisions for hypertensive patients in daily practice.
The reduction in BP with ARB treatment reported across the different observational studies in this review appears to be comparable for the different agents. However, direct comparisons cannot be made owing to different durations of treatment (from 3 to 9 months) and differences in patient groups at baseline, for example different CV risk parameters and CV disorders. Of the observational studies on ARBs reviewed in this article, the POWER study with over 29,000 patients was the largest.
Selection of Cardiovascular Risk Assessments
Advantages of SCORE
There are many advantages of using SCORE to calculate CV risk in patients. SCORE provides clinicians with a practical approach to identify those patients at high risk of a fatal cardiovascular event; the colour-coded SCORE risk charts are in a simple format that makes it easy for clinicians to estimate CV risk using routine clinical measurements [8]. Furthermore, SCORE is available as an electronic version that can be used online or downloaded from the website (www.heartscore.org).
SCORE was derived from 12 European cohort studies with a total of 205178 patients representing 2.7 million person years of follow-up [8]. It uses SBP to estimate total CV risk and there is evidence to suggest that SBP rather than DBP is a better predictor of CV events [20]. Since its derivation, SCORE has been validated in numerous external studies in different countries and has shown good discrimination between people at high and low risk of a cardiovascular event [21]. SCORE can also be adapted for country-specific use; SCORE risk charts are available for high-risk and low-risk European countries [8] and this tool has also been successfully calibrated for use in individual countries [22, 23].
Limitations of SCORE
A limitation of SCORE is that it only takes into consideration principal risk factors; other risk factors, such as a strong family history of early-onset CV disease, milder degrees of impaired glucose regulation, triglyceride levels and fibronectin, should also be considered [8]. Another limitation of SCORE, also noted for other risk scores, is that the effect of other medication (on CV risk) is not fully assessed and adjusted for. Ideally, medication used prior to the study and medication started during the study follow-up should be factored into the SCORE risk charts [24].
Some studies have demonstrated that SCORE may underestimate CV risk in specific patient groups. Szyndler and colleagues demonstrated that, when compared with the ESC/ESH hypertension guidelines, SCORE underestimated the burden of CV risk among hypertensive patients, particularly women [25]. Furthermore, a comparison of SCORE with the Framingham-D’Agostino CV scale revealed that SCORE may underestimate CV risk in men who have an unfavourable blood lipid profile [26].
Role of Framingham Risk Assessment
The Framingham risk algorithm was originally derived from participants of the Framingham Heart Study in the USA (1971-1974) which included 2489 men and 2856 women [9]. It has been assessed and validated in numerous external studies and has shown good discrimination between high- and low-risk patients [21]. The Framingham risk score may be more suitable for use in a North American population, including in Canada. Indeed, Grover and colleagues have demonstrated that the Framingham risk score was able to show good discrimination in a Canadian cohort [27].
CLINICAL INSIGHTS FROM OBSERVATIONAL STUDIES OF ARBs
The observational studies reviewed here confirm that ARB-based therapy reduces SBP and DBP in large, unselected primary care populations. Reduction of SBP has been previously correlated with regression of left ventricular hypertrophy and improvement of CV outcomes [28-32]. A proportion of these observational studies also reported a benefit of ARBs on total CV risk [10-14, 17, 18], a measure recommended by the ESC/ESH guidelines published in 2013 [4]. In particular, the POWER study confirmed that physicians can use SCORE accurately to assess total CV risk, as shown by the comparisons of recorded and calculated SCORE risk [11]. Results from the POWER study, the BSCORE and EXCELLENT studies in the valsartan translational research programme, and the candesartan CHILI Triple T study demonstrate the importance and value of measuring total CV risk before and after treatment, suggesting that these assessments should be performed in future CV studies.
New healthcare practices, such as the use of EHRs, will facilitate observational studies in much larger patient populations. Algorithms embedded in EHR systems will serve to inform patient care and will continuously evolve in agreement with clinical observations and new research. These algorithms will be derived entirely from large pools of data, making it possible to draw conclusions from observed trends. In the future, it is anticipated that these algorithms will evolve as decision support tools to enable large observational studies to be conducted with less direct involvement of physicians and less inconvenience for the patient.
CONFLICT OF INTEREST
The author confirms that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
The author acknowledges editorial support provided by Adelphi Communications Ltd, UK, supported by Abbott Products Operations AG, Allschwil, Switzerland.
The development of this article was supported by an unrestricted educational grant from Abbott Products Operations AG, Allschwil, Switzerland. Abbott had no control over the content of this review and Professor Goudev received no payment for any part of his work on this article.
PATIENT’S CONSENT
Declared none.


