All published articles of this journal are available on ScienceDirect.
Hawk´s Beak Form in Midventricular Takotsubo Syndrome: Two Case Reports from Latin America
Abstract
Takotsubo syndrome is a type of acute reversible heart failure that can involve a form of acute catecholaminergic myocardial stunning. This clinical entity shows a pattern of temporary left ventricular dysfunction in the absence of occlusion of any coronary artery. A midventricular type is a form of Takotsubo syndrome where the atypical morphological variant is Hawk’s beak. The prevalence of this type is estimated to be 10-15% in several series in Asian and Western countries (predominantly Caucasian patients). In Latin America, there are no studies reporting this type of presentation. Two cases are reported in women initially diagnosed with acute myocardial infarction with the finding of the atypical hawk's beak morphology of Takotsubo syndrome, confirmed by left ventriculography. One of them was followed up early, observing recovery in her ventricular function without structural compromise at the level of contractility and with a good response to the outpatient treatment proposed. As there is a low prevalence and few published reports, these 2 cases are presented to promote long-term studies and increase the information regarding the evolution and morbidity/mortality of this type of presentation compared with the classical form of the syndrome.
1. INTRODUCTION
Takotsubo syndrome was introduced in 1990, who published 5 cases of patients who showed the unusual aspect of the left ventricle at the end of systole, which resembles a trap to capture octopuses in Japan [1]. These patients reported chest pain and electrocardiogram characteristic of acute myocardial infarction without coronary artery lesions [1]. The hawk's beak form, one of the atypical types characterized by mid-ventricular motility anomaly, was first described by Roncalli et al. (2007). However, Hurst et al. (2006) reported 4 case series with clinical characteristics and transient nature suggested sharing a pathophysiological mechanism like the classical type [2], but without a clear explanation about the unique involvement of the mid-ventricular region. Although progress has been made in the knowledge of this entity, given the recent progress in the understanding of its physiopathology, the long-term outcome of the condition continues to be controversial. Currently, there is no report of this variant in the Latin American population. We report 2 cases admitted with the suspicion of an acute coronary syndrome in 2 Colombian women.
2. CASE REPORT 1
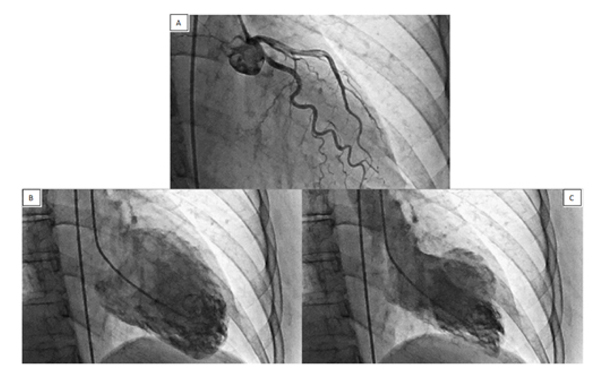
A 57-year-old woman was admitted to the coronary intensive care unit after presenting a sudden episode of severe retrosternal pain at rest radiating to her neck and upper limb accompanied by nausea. The pain started after receiving stressful news related to the stabbing injury of her child. The medical history included gallbladder cancer in remission and second-hand tobacco smoke. She was normotensive with no signs of low output. The electrocardiogram showed sinus bradycardia with q-wave plus t-wave inversion from v1 to v3. Laboratory studies revealed an elevated troponin T level based on the 99th percentile as the cutoff value. Transthoracic echocardiogram demonstrated hypokinesia in the middle third antero-septal region of the left ventricle and 56% ejection fraction. These findings were considered compatible with acute coronary syndrome, for which antithrombotic and antischemic therapy was administered, but the coronary angiography reported normal coronaries. However, the left ventriculography showed apical and mid-ventricular hypokinetic with normally contracting heart base compatible with Takotsubo syndrome type mid-ventricular hawk's beak form (Fig. 1). The patient progressed without signs of heart failure and was discharged after 2 days of hospitalization with pharmacological treatment consisting of angiotensin converting enzyme inhibitors, beta-blocker, and statin. Not antiplatelet agent due to not having cardiovascular risk factors and absence of atherosclerosis.
3. CASE REPORT 2
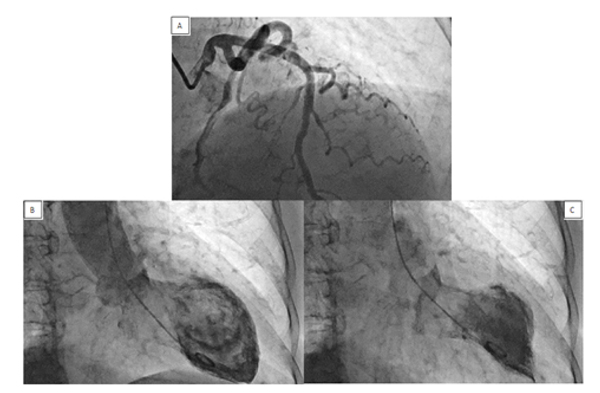
An 80-year-old woman admitted to the cardiology clinic with symptoms of sudden onset of pain in the precordial region radiating to the left upper limb and jaw, associated with dyspnea, nausea, and sensation of palpitations. Her medical history included high blood pressure, type 2 diabetes mellitus and chronic obstructive pulmonary disease. The patient expressed that a few hours before, she had a strong argument with her family. During the evaluation, the patient presented as a hypertensive emergency accompanied with angina that was treated with vasodilator infusion. Electrocardiogram showed Q wave in leads v1 to v4 and T wave inversion from v1 to v6. Her laboratory studies revealed elevated troponin I level based on the 99th percentile as the cutoff value. The findings of the transthoracic echocardiogram showed contractility alterations given by mild lateral hypokinetic and 45% ejection fraction. Left heart catheterization was performed, demonstrating incipient atherosclerotic disease of the right coronary artery (non-dominant vessel). The left ventriculography showed papillary muscle hypertrophy, apical and mid-ventricular hypokinetic with hawk´s beak form (Fig. 2). The patient progress of was discharged after 72 h of hospital management with pharmacological treatment angiotensin converting enzyme inhibitors, beta-blocker, statin, antiplatelet agent, metformin, and anticholinergic bronchodilator. Twenty days after the event, another transthoracic echocardiogram was performed, reporting 57% left ventricular ejection with mild aortic and mitral insufficiency, but without alterations in global or segmental contractility. These findings coincide with the characteristics of transient ventricular dysfunction and improvement in contractility disorders, reported so far in the literature regarding this variant of Takotsubo syndrome.
4. DISCUSSION
Takotsubo syndrome is an acute cardiac disease entity with a clinical presentation resembling that of an acute coronary syndrome. The syndrome has been increasingly recognized in almost all countries [6]. It is uncommon in Hispanics and in Latin America [1]. This clinical entity is also known as stress-induced reversible cardiomyopathy, broken heart syndrome or apical ballooning syndrome and is characterized by remarkable apical akinesia leading to acute transient systolic dysfunction in the absence of significant coronary artery disease. Typically, these patients are postmenopausal women (80%) who exhibit mild to moderate chest pain, ST segment elevation in the v 3 to v6 leads, and a modest increase in cardiac markers [3].
Previous studies have reported that 95% of all patients with Takotsubo syndrome survive the acute syndrome with the recovery of cardiac function and with an extremely rare incidence of recurrence. However, there are no specific studies for the atypical hawk's beak form, only a few case series reports [3]. Therefore, this syndrome should be considered in the differential diagnosis for postmenopausal women with findings suggestive of acute myocardial infarction and a history of physical or mental stress preceding the symptoms [4]. We reported two cases of Colombian women with signs and symptoms related to a trigger factor such as emotional stress with a hawk's beak appearance seen on ventriculography. In the typical Takotsubo syndrome, the left ventricle usually takes the form of an octopus trap. However, there is an atypical form of the mid-ventricular type of the Takotsubo syndrome where hypercontractility of the apical region and dyskinesia of the medium ventricular cavity is identified along with a normally contracted base [5]. This test shows a specific sign in the apex of the left ventricle to identify this characteristic as an anatomical variant. The prevalence of hawk's beak is estimated to be 10-15% in several series in Asian and Western countries (predominantly Caucasian patients) [6]. In Latin America, there are no reports of this anatomical form of presentation.
The specific etiology of this variant is not yet completely clear, but the transient dysfunction may be secondary to microvascular spasm or regional myocarditis like that presented in the typical form [6]. In addition, possible mechanisms have been described as multivessel epicardial spasm, acute coronary syndrome with reperfusion, alteration of fatty acid metabolism, transient obstruction at the exit of the left ventricle (LV) and catecholamine-mediated myocardial dysfunction [7]. Probably a complex interaction between catecholamines and the adrenergic innervation of the heart occurs. These hypotheses, formulated by Lyon et al., suggest a toxic effect on cardiomyocytes [8, 9]. Studies in animal models demonstrated that the activation of alpha and beta adrenoreceptors is the main trigger of cardiac changes induced by emotional stress [8]. The greater amount of adrenergic beta 1 (B1) and beta 2 (B2) receptors in the apical region compared with the basal zone has been proven in stress cardiomyopathy. Additionally, in the LV there is an inverse distribution of the sympathetic nerve endings indicate that the sympathetic innervation is greater at the base than at the apex [9]. This would imply a greater apical response to circulating epinephrine, coming from the adrenal medulla, which would compensate for the reduced apical sympathetic innervation. This innervation would guarantee a harmonic contractile response of the LV in response to stress [9].
The long-term mortality (average 28 months) for Takotsubo syndrome is 3.5% [10] and for the hawk's beak variant, we believe that there is still much to elucidate. In our cases, a patient was followed up early, observing recovery in her ventricular function without structural compromise at the level of contractility and with a good response to the prescribed outpatient treatment.
CONCLUSION
In conclusion, there are few studies to establish the complications and mortality rate of the hawk's beak variant compared with the general population and typical Takotsubo syndrome. It is important to consider Takotsubo syndrome as a differential diagnosis of acute coronary syndrome and thus increase the reporting of patients with this atypical form and increase our knowledge about its clinical evolution and prognosis.
AUTHORS' CONTRIBUTIONS
All the authors were involved in writing and revising the article prior to submission.
ETHICAL STATEMENT
The author confirms that the requirement for ethical approval was waived off by the Hemodynamic and Interventional Cardiology Department, Heart institute of Bucaramanga Headquarters Bogota.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patients.
STANDARDS OF REPORTING
CARE guidelines have been followed in this study.
FUNDING
The authors have no financial relationship with any commercial entity relevant to the subject of this manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest in association with the present study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the finding of the article is available in the Zenodo Repository at zenodo.org, reference number http://doi.org/10.5281/zenodo.5081353.
ACKNOWLEDGEMENTS
Declared none.


