All published articles of this journal are available on ScienceDirect.
Endovascular Surgery or Both: A Case Report of Hybrid Procedure in a Patient with Abdominal Aortic Aneurysm and Tasc D Aortoiliac Occlusive Disease
Abstract
Hybrid procedure, a combination of endovascular and open surgical approach, has emerged as the first-line treatment for patients with severe aortoiliac diseases because of its effectiveness. We report a hybrid procedure in a 72 year old man with an Abdominal Aortic Aneurysm (AAA) and Trans-Atlantic Inter-Society Consensus (TASC) D aortoiliac occlusive disease. After two failed attempts using the intraluminal technique (retrograde and antegrade), we successfully performed an endovascular approach with subintimal and Subintimal Arterial Flossing Antegrade-retrograde Intervention (SAFARI) technique with the help of roadmap technology. The vascular surgeon completed the procedure by creating femorofemoral bypass using a Great Saphenous Vein (GSV) graft. The graft was patent and there were no complications at 1 week, 1 month and 6 months follow-up.
1. INTRODUCTION
The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial answered the debate regarding the best treatment for the aortoiliac disease [1]. Both endovascular and open surgical approaches had similar outcomes in terms of amputation-free survival but the endovascular approach was superior because, in the short term, the surgical approach was more expensive [1]. However, not all aortoiliac disease can be treated with the endovascular or open surgical approach alone. Therefore, hybrid procedures emerged as another option to treat the chronic total occlusion. The 2017 European Society of Cardiology (ESC) guidelines on diagnosis and treatment of Peripheral Arterial Diseases (PAD) recommend hybrid procedures for the management of the aortoiliac disease [2]. We report a case of a 72-year-old male with an Abdominal Aortic Aneurysm (AAA) and Trans-Atlantic Inter-Society Consensus (TASC) D aortoiliac occlusive disease who successfully underwent a hybrid procedure.
2. CASE PRESENTATION
A 72-year-old Chinese male presented to the emergency room with sudden abdominal to buttock pain and claudication of both lower extremities. No chest pain or dyspnoea was reported. The patient was previously admitted for melena and colon cancer. The patient had a history of hypertension and was a smoker. A “bump” was found during the physical examination focused at the centre of the abdomen. The ankle-brachial index of both lower extremities was 0.7 and the pulse of both femoral arteries was weak.
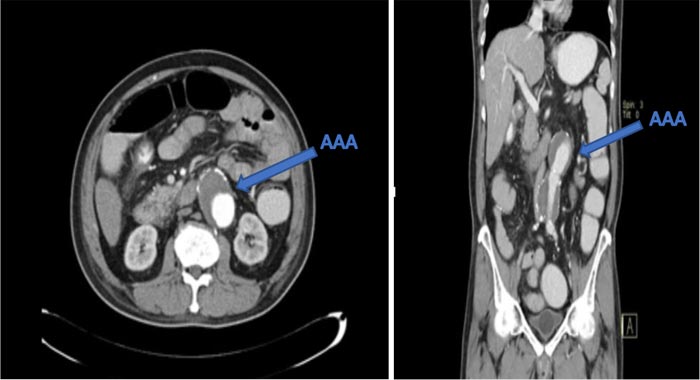
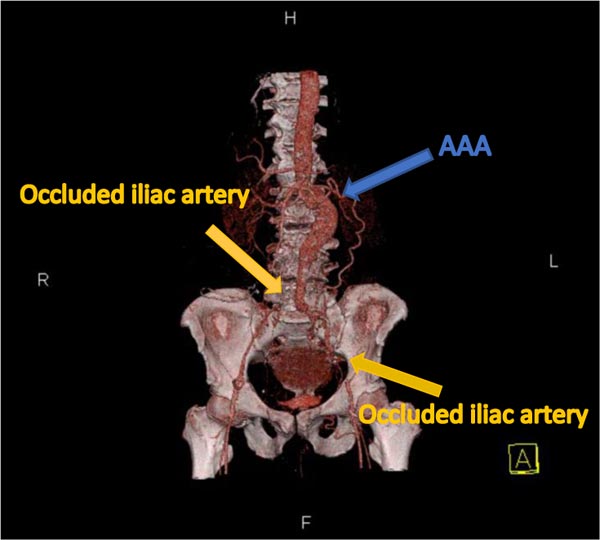
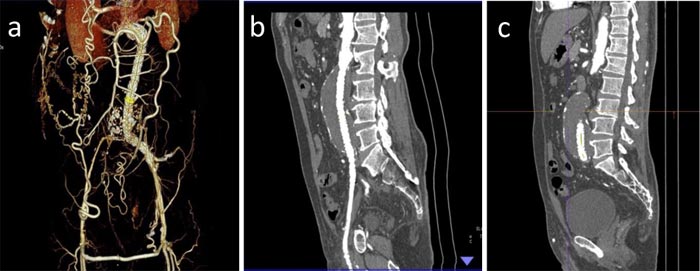
The initial electrocardiogram and chest X-ray of the patient were normal. The initial serum creatinine level was 0.9 mg/dL (normal range: 0.7-1.2 mg/dL). Endoscopic examination showed that the patient has large oesophageal varices. Echocardiography showed normal Left Ventricular (LV) function and did not reveal any sign of regional wall motion abnormalities. Computerized Tomography (CT) angiography showed enlargement of the abdominal aorta with no dissection and retroperitoneal leak (Fig. 1); 3D CT angiography confirmed the CT angiography findings. Furthermore, both common iliac arteries were totally occluded (Fig. 2).
Four major problems were present in this patient; elderly, high risk of bleeding from the oesophageal varices, high risk of developing renal failure, and high mortality rate. A clinical meeting was conducted involving the interventionist, gastroenterologist, vascular surgeon, and anaesthesiologist. Three options were discussed; surgical approach, endovascular approach, and hybrid procedure (a combination of both surgical and endovascular approaches). Pursuing the surgical approach was a very high-risk option because of the patient’s age and the high risk of bleeding. It was also likely to be associated with more complications, long-term hospitalization, and a high mortality rate. On the other hand, an endovascular approach (for the combination of AAA and TASC D aortoiliac occlusive disease) was considered too complicated, with a high risk of rupture and a high mortality rate. The benefits of a hybrid procedure include more rapid recovery and less risk of complications. These will result in short term hospitalization and a lower mortality rate. The cost of each procedure varies, with the hybrid procedure needing the highest cost and the surgical the lowest. The patient and the family received an explanation of the expected outcome, risks, and complications of the alternatives in a separate meeting, and opted for the hybrid procedure.
3. INTERVENTION
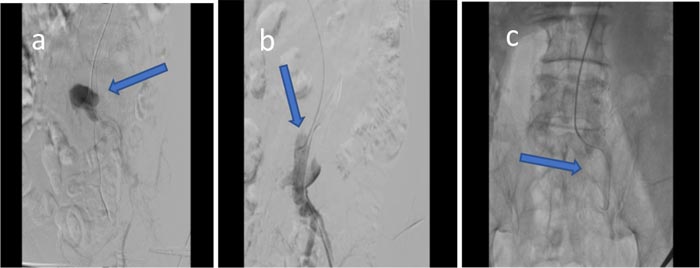
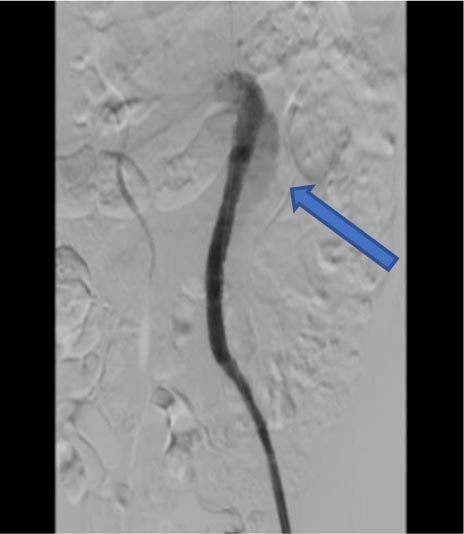
A 6 Fr sheath was inserted from the left brachial artery and another access was made from the left femoral artery. The first attempt used intraluminal and subintimal technique in combination with buddy balloon or buddy with guiding catheter technique along with retrograde approach made from the left femoral artery with Glidewire (GW) Terumo hydrophilic 035/GW ES Command 018 (Terumo, Tokyo, Japan). However, the attempt was unsuccessful because the catheter reached the false lumen (Fig. 3a). The second attempt employed the antegrade approach from the left brachial artery using the same instrument. This attempt was unsuccessful because the catheter entered the collateral and false lumen (Figs. 3b and 3c).
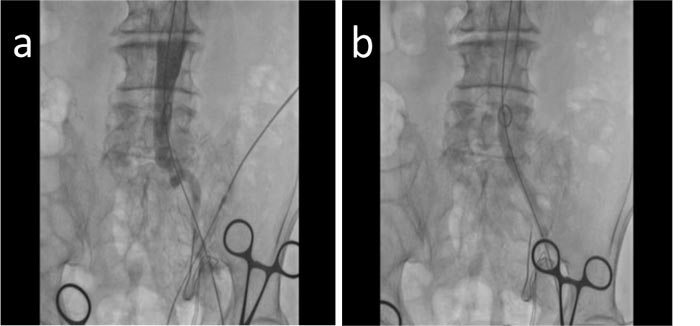
The final attempt used both an antegrade and retrograde approach with the help of roadmap technology. This technique is known as the subintimal arterial flossing antegrade-retrograde intervention (SAFARI) technique. The antegrade wire from the left brachial artery used the subintimal technique to pass the thrombus, while the retrograde wire from the left femoral artery used the intraluminal technique. We used contrast to check the wire position. After we confirmed that it was placed correctly intraluminally proximally and distally of the lesion (Fig. 4a), we performed pre-dilatation (Fig. 4b). Afterward, we inserted a multipurpose catheter DC MP 6 Fr (Terumo, Tokyo, Japan) from the left femoral artery. We changed the wire from GW Terumo Hydrophilic to Lunderquist (Cook Medical, Bjaeverskov, Denmark). We performed another contrast injection to ensure that the wire was in a straight position intraluminally and linear to the aortic-iliac femoral line. Then, we deployed the first endovascular (EVAR) graft 32.0/100 (Medtronic, Inc., Santa Rosa, USA) in the abdominal aorta, followed by the second EVAR graft 12.0/100 (Medtronic, Inc., Santa Rosa, USA) from the abdominal aorta to the ostium of the common iliac artery, and third EVAR graft 12.0/80 (Medtronic, Inc., Santa Rosa, USA) from the ostium of the common iliac artery to the distal of the common iliac artery until the external iliac artery has been reached. After dilating the vessel with the EVAR graft, we inserted the balloon 20.0/46 (Medtronic, Inc., Santa Rosa, USA) from proximal until reaching the distal part of the graft. There was a small type 1b endoleak found during contrast injection (Fig. 5). Finally, the vascular surgeon created an anastomosis bypass from the left femoral artery to the right femoral artery using the right great saphenous vein that had been prepared before.
4. EVALUATION AFTER THE PROCEDURE
The patient underwent hospitalization for a total of 4 days before being discharged. Bleeding and acute kidney injury occurred after the procedure. The haemoglobin dropped from 9.5 to 5.4 g/dL (normal range: 13.5-17.5 g/dL) but we managed to restore it to 11.0 g/dL on the fourth day. The serum creatinine increased from 0.9 to 2.98 mg/dL, but it decreased to 1.2 mg/dL on the fourth day. The changes in serum creatinine was a contrast-induced acute kidney injury (CI-AKI) due to the contrast (200 mL Iopamirol) that we administered during the intervention procedure. CI-AKI occurred even though we have taken preventive measures by hydrating the patient with saline (500 mL), 3 h prior to the procedure. No acute limb ischaemia, perforation, infection, and other complications were observed after the procedure. The patient was scheduled for 1 week, 1 month, and 6 months follow-up after being discharged. During the follow-up, the sealing was good and there was no endoleak (Fig. 6).
5. DISCUSSION
AAA and aortoiliac disease occur in elderly smokers [3]. The previous trials recommend endovascular procedures as first-line treatment in patients with aortoiliac disease because of their superiority compared with open surgical procedures [1, 4]. In this case, our patient was a 72-year-old male with a history of smoking as well as AAA and TASC D aortoiliac occlusive disease. Our multidisciplinary team discussed the alternatives and concluded that an endovascular procedure alone was not suitable and decided on a hybrid procedure. Hybrid procedure is not uncommon in treating a patient with severe aortoiliac disease; up to 24% of patients with TASC C and D lesions needed to be treated using this procedure [4]. Previous studies reported the primary success rate of a hybrid procedure to be as high as 93-100% [5]. Furthermore, patients treated with the hybrid procedure have shorter hospitalization duration and less morbidity compared with open surgery [6]. Due to the severity of aortoiliac disease in this patient (AAA and TASC D) and the benefits of the procedure, the clinical team suggested a hybrid procedure as the definitive treatment.
The hybrid procedure began with the endovascular approach. The attempt to cross the lesion can be started with a retrograde approach via the femoral artery and if it does not result in being successful, an antegrade approach via the brachial artery could be attempted [4]. The intraluminal technique was performed prior to the subintimal technique because, if successful, its response to the balloon was more favourable, but it took more time [7]. The subintimal technique is known for its superiority in long occlusions and patency because it is faster, and has a higher technical success, as well as high limb salvage rates [8, 9]. The false lumen created by this technique rarely develops into recurrent stenosis because it does not consist of endothelium and atheroma. The subintimal recanalization also positively affects the collateral. It was reported from the previous study that new collaterals were found after the subintimal recanalization [8]. In performing the endovascular approach, we tried both approaches (retrograde and antegrade) with both techniques (intraluminal and subintimal) and still failed because we kept on reaching the collateral and false lumen instead of true lumen. Our next step was to perform the SAFARI technique. This technique helped interventionists in the setting where the conventional antegrade intraluminal approach failed to cross the chronic occlusion or when a limited distal artery was available for re-entry [10, 11]. We approached the lesion from an antegrade and retrograde direction at the same time with the help of roadmap technology. Roadmap technology was important during peripheral intervention procedure because it helped to visualize the vessels and the precise position of the stent with less use of contrast [12]. The retrograde wire via the left femoral artery crossed the lesion with the intraluminal technique, while the antegrade wire via the left brachial artery crossed the lesion via the subintimal technique. The attempt using the SAFARI technique was successful and 3 EVAR grafts were deployed.
The endovascular procedure successfully restored the arterial blood flow in the left extremity. The next step was to restore the arterial blood flow in the right extremity with a surgical procedure. In the long term, femorofemoral crossover bypass brought good outcomes when applied to patients with unilateral iliac diseases [13]. In this case, we used the great saphenous vein (GSV) for femorofemoral graft instead of an artificial graft because of its effectiveness. The GSV was better in 3 years primary patency rate compared with polytetrafluoroethylene grafts [14]. Furthermore, GSV was less expensive compared with an artificial graft. The hybrid procedure restored the arterial blood flow to both lower extremities and was evaluated for patency until 6 months of follow-up. In a previous study, during a mean follow-up of 4 years, the patients who underwent unilateral iliac stenting and femorofemoral crossover bypass were symptom-free and had patent grafts [15]. Further follow-up will be carried out in this patient to evaluate symptoms and the patency of arterial blood flow in both lower extremities.
CONCLUSION
Interventionists and vascular surgeons should consider the hybrid procedure as the first-choice treatment for complex aortoiliac disease because of its good short and long-term outcomes, fewer complications, and shorter length of hospital stay. However, the higher cost of this procedure compared with the endovascular and open surgical approach should be taken into consideration. The use of roadmap technology, subintimal technique, and SAFARI technique is beneficial for the endovascular approach in treating chronic total occlusion of the iliac artery. While for the open surgical approach, femorofemoral crossover bypass can be carried out to restore the blood flow in the contralateral extremity and a GSV graft is more effective, patent, and less expensive compared with artificial grafts. Finally, good collaboration in a multidisciplinary team will produce a good outcome and help solve complicated cases.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by Research Ethics Committee Medicine and Health University School of Medicine Muhammadiyah Prof. Dr. Hamka, Indonesia with approval number KEPKK/FK/09/2020.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient.
STANDARD OF REPORTING
CARE guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank all who supported this case report.


