All published articles of this journal are available on ScienceDirect.
Bridging with Tirofiban During Temporary Withdrawal of Oral Antiplatelets for Two Major Surgical Procedures in High Ischaemic Risk Patients
Abstract
Background:
Recent coronary stent implantation requires Dual Antiplatelet Therapy (DAPT) for at least 6 months. Serious issues are raised when non-cardiac surgery is required during this period, because of the balance between ischemic and haemorrhagic complications.
Case Reports:
We report 2 high ischemic risk cases requiring intermediate bleeding risk non-cardiac surgery, during the first month of DAPT initiation. Perioperative management with discontinuation of the P2Y12 inhibitor and bridging with tirofiban, while aspirin was uninterrupted, was uneventful.
Conclusion:
Bridging with intravenous glycoprotein IIb/IIIa receptor inhibitors may be a safe and effective alternative to P2Y12 inhibitor discontinuation in non-deferrable non-cardiac surgery.
1. INTRODUCTION
The European Society of Cardiology (ESC) Guidelines recommend Dual Antiplatelet Therapy (DAPT) using aspirin and a P2Y12 receptor inhibitor for 6 months, following an Acute Coronary Syndrome (ACS) with coronary stent implantation. However, when a patient is on DAPT and needs urgent surgery within these 6 months, DAPT raises issues. Interruption of a P2Y12 receptor inhibitor is recommended for 3-7 days prior to surgery to enable recovery of platelet function and eliminate the potential risk of peri- and post-procedural bleeding. On the other hand, early cessation of antiplatelet therapy has been related with cardiac ischaemic complications and these patients are considered as being at high ischaemic risk [1-4].
2. CASE REPORTS
We present 2 cases of patients who were on DAPT after an ACS and needed surgery within a month after stent implantation.
A 79-year old male patient, with diabetes mellitus, arterial hypertension and a previous medical history of Coronary Artery Bypass Grafting (CABG) (LIMA to the LAD, SVG to the RCA) 20 years ago, was admitted with a Non-ST Segment Elevation Myocardial Infarction (NSTEMI). He underwent percutaneous coronary intervention with a zotarolimus drug-eluting stent (Resolute Integrity™, Medtronic, Minneapolis, USA) implantation in the venous graft of the right coronary artery and was discharged haemodynamically stable, on DAPT, aspirin 100 mg q.d. and clopidogrel 75 mg q.d. Twenty days later, he was readmitted with lower gastrointestinal bleeding. Colonoscopy revealed a malignant mass in the sigmoid colon and surgical resection was decided. This was a high thrombotic and intermediate haemorrhagic risk surgical procedure and therefore, we decided to stop clopidogrel and bridge with tirofiban [4].
A 69-year old male patient, smoker and hypertensive, was admitted with an inferior ST- Elevation Myocardial Infarction (STEMI). He underwent a primary percutaneous coronary intervention with a zotarolimus drug-eluting stent (Resolute Integrity™, Medtronic, Minneapolis, USA) implantation in the right coronary artery and was started on DAPT, aspirin 100 mg q.d. and ticagrelor 90 mg b.i.d. During hospitalization a malignant pulmonary mass was discovered incidentally and pneumonectomy was decided. This was considered a high thrombotic and intermediate haemorrhagic risk surgical procedure and therefore, we decided to stop ticagrelor and bridge with tirofiban [4].
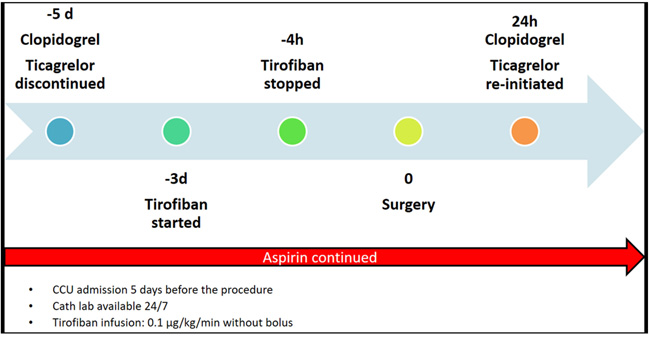
For the first patient, clopidogrel was discontinued 5 days before surgery, and for the second patient, ticagrelor was discontinued 5 days before surgery (Fig. 1). Both patients were admitted to the coronary care unit 5 days before the procedure and tirofiban infusion was initiated after 48 h at a dose of 0.1 μg/kg/min without bolus [5]. Haemoglobin, haematocrit and thrombocytes were checked before starting, 6 h after starting intravenous tirofiban, and daily thereafter. Prothrombin Time (PT), activated Partial Thromboplastin Time (aPTT), kidney and liver function tests were within normal limits. Tirofiban treatment was interrupted 4 h before surgery.
3. RESULTS
Both surgical procedures were uneventful and clopidogrel and ticagrelor were resumed respectively in the 2 patients 24 h after surgery. The histological examination was positive for a colon adenocarcinoma in the first patient and a pulmonary adenocarcinoma in the second one. Both patients were discharged on DAPT and haemodynamically stable, without any cardiac ischaemic complications after a follow-up of 6 months.
4. DISCUSSION
Tirofiban is a non-peptide tyrosine derivative and inhibits platelet aggregation by attaching to the glycoprotein IIb/IIIa receptor. Its plasma half-life is 1.6 h and platelet function recovers within 4 h after cessation of administration [6, 7]. Renal excretion accounts for 65% of its plasma clearance [8]. Tirofiban can cause severe but reversible thrombocytopenia due to an immunologic mechanism provoked by antibodies against the structure created by the glycoprotein IIb/IIIa receptor and the attached tirofiban. Tirofiban-induced thrombocytopenia is usually managed with suspension of the drug, as it is removed from the circulation within the first hours of its discontinuation [9].
Patients who are on DAPT after coronary stent implantation and will need non-cardiac surgery, require a multidisciplinary decision (by cardiologists, interventional cardiologists, anaesthetists, haematologists and surgeons), regarding stratification for thrombotic and bleeding risk. Possible stent thrombosis, in case DAPT has to be stopped, possible peri- and post-procedural bleeding in case DAPT cannot be stopped and the effects of postponing surgery should be taken into consideration [1, 4].
The thrombotic risk is classified as low, intermediate and high depending on the duration after the coronary stent implantation and other stent-driven high-risk features, as described in detail by Rossini et al. [4]. The aforementioned authors provide detailed tables, useful for decision-making in each kind of surgical procedure based on the haemorrhagic and thrombotic risk [4]. A high risk of major adverse cardiac events has been reported, if non-cardiac surgery is performed within the first weeks after coronary stent implantation. Apart from DAPT cessation, surgery can have pro-inflammatory and prothrombotic effects, and as a result, the risk of coronary thrombosis, even at the level of the stented coronary segment is increased [3].
When the bleeding risk is high and the patient is on DAPT, as it happens in vascular reconstructions, complex visceral procedures, neurosurgery, and transbronchial operations, timing of P2Y12 cessation has to be optimal to reduce the off-therapy period before surgery. Regarding aspirin, in most cases, the benefit of its use outweighs the risk and should be continued, except for procedures with extremely high bleeding risk, like intracranial procedures, transurethral prostatectomy or intraocular procedures [3, 4].
For patients with a very high risk of stent thrombosis, bridging therapy with intravenous, reversible glycoprotein inhibitors, such as eptifibatide or tirofiban is an alternative to P2Y12 cessation. The P2Y12 inhibitor should be reinitiated within 48 h after surgery, taking into consideration the thrombotic risk in patients with recent coronary stenting [4, 5]. Such surgical operations should be performed in hospitals where catheterization laboratories are available 24/7, so as to treat patients immediately in case of perioperative thrombotic events [1].
The reported patients underwent surgical procedures with a simultaneous intermediatebleeding and high-ischaemic risk, as surgery was performed within the first month following coronary stenting for ACS. Therefore, bridging with tirofiban was deemed necessary prior to the operation and the P2Y12 inhibitor was restarted within 24 h after surgery. Aspirin was continued without interruption. Neither bleeding nor ischemic complications occurred for both patients peri-operatively and within a 6-month follow-up period.
Patients who are scheduled to undergo stent implantation should be carefully informed about the bleeding consequences of a rather prolonged DAPT therapy and the possible thrombotic complications in case surgery is required and DAPT should be discontinued. However, this is not always applicable, especially in cases where stent implantation is performed in the setting of an ACS, as described in our cases.
CONCLUSION
A comprehensive assessment of bleeding and ischaemic risks is required in patients who will undergo a non-cardiac surgery, early after coronary stent implantation. Bridging with intravenous glycoprotein IIb/IIIa receptor inhibitors may be a safe and effective alternative to P2Y12 inhibitor discontinuation if non-deferrable surgery is required. The role of a multidisciplinary team and the performance of such surgical procedures in hospitals where catheterization laboratories are available 24/7 are essential.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Informed consent have been obtained from all the participants.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


