All published articles of this journal are available on ScienceDirect.
Local Use of Ankaferd Blood Clotter in Emergent Beating Heart Coronary Artery Bypass Grafting
Abstract
Background:
Severe beeding which requiring massive blood transfusion after emergent beating heart surgery is shown to be 1–3%. Therefore, complications and side effects of transfusion can be seen. The aim of this study was to investigate the effectiveness of Ankaferd blood clotter (ABC) as a new topical herbal blood clotter to decrease mediastinal bleeding in emergent beating heart CABG patients who medicated with clopidogrel and acetyl salisilic acite (ASA) prior to CABG surgery.
Materials and Methods:
25 CABG patients received a high dose clopidogrel (600 mgr) and 300 mgr ASA have been included into the study (ABC group). 25 patients have also been included into the study for comparison (placebo group, PG). After the administration of protamine sulphate, a 10 ml of ABC solution has been sprayed to the surgical area including mediastinum and epicardial sac. We compared mediastinal drenaige, reoperation due to tamponade, and required blood and blood products in both groups.
Results:
The mean amount of bleeding after operation was 230 ml in ABC group, and 490 ml in CG (P=0.001). In ICU, bleeding in ABC group and CG was 410ml and 680ml, respectively (P=0.0022). The mean total bleeding from mediastinum was 530±280 mL and 990±440 mL In ABC and CG group, respectively (P=0.001). The amount of autotransfusion was as follows: 175 mL in ABC group, and 290 mL in CG (P=0.002). No patient needed the surgical revision in ABC group, but four patients (16%) from CG group because of cardiac tamponade. Seventeen patients from CG required blood transfusion due to low hematocrite level postoperatively. In CG, the mean hematocrite level was 17±2,3. Transfusion of fresh frozen plasma and platelets in ABC group and CG were as follows: 0.2 and 0 in ABC group, and 0.3and 0.4 in CG.
Conclusion:
Our study showed that the local use of 10 mL ABC reduces bleeding significantly. Therefore, transfusion requirements of PRBC, platelets, and total blood units in patients on clopidogrel and ASA undergoing emergent beating heart CABG. To provide cardiac tamponade because of excessive mediastinal bleeding and requirement of blood transfusion after emergent CABG patients who previously administered clopidogrel and ASA, we propose local use of ABC solution as a potent coagulant agent.
Introduction
The reoperation rate because of excessive bleeding after emergent on-pump cardiac surgery is shown to be 3-5%[1-3]. Transfusion of allogeneic blood products exposes the patient to additional risks such as transfusion reactions, viral transmission, immunosuppression, and increased mortality rates and increases the cost of the procedure [2]. Risk factors are longer operation time, five or more grafts anastomosis, antiaggregant and anticoagulant use prior to surgery. Thus, as we know that reoperated patients have a three to five times greater mortality [3]. As a result of reexploration, morbidity regarding renal and pulmonary function, sepsis and arrhythmia have been reported [5]. Postoperative excessive bleeding may be due to surgical or hematologic reasons. A high dose of ntiplatelets thrapy prior to coronatry angiography such as aspirin and clopidogrel are frequently used in a number of unstable coronary artery disease (CAD) patients. Many of whom are receiving heparin infusions, and varying practices with regard to the use of antifibrinolytic drugs which is the risk factors of postoperative bleeding. Clopidogrel treatment a class I recommendation with grade A evidence in CAD patients. Current guidelines support the discontinuation of clopidogrel 5 to 7 days before CABG.
Ankaferd blood clotter is composed of a standardized mixture of the plants Thymus vulgaris, Glycyrrhiza glabra, Vitis vinifera, Alpinia officinarum, and Urtica dioica. All of those plants individually have some effects on the endothelium, blood cells, angiogenesis, cellular proliferation, vascular dynamics and mediators [6-9]. Recently, Goker et al. have demonstrated the basic mechanism of Ankaferd Blood Clotter [ABC] as a new haemostatic drug [10]. They have shown that ABC have induced a very rapid formation of a protein network within the plasma and serum [10].
| ABS(n =25) | PG | P | |
|---|---|---|---|
| Male/female | 16/9 | 15/10 | 0.94 |
| Age (years) | 44.2 (37.4-61.8) | 46.4 (38.3-59.5) | 0.89 |
| Last clopidogrel intake before surgery | |||
| < 24 hours | 11 | 12 | 0.92 |
| [ΙΝΣΕΡΤ ΦΙΓΥΡΕ 004]≥ 24 < 48 hours | 14 | 13 | 0.94 |
| The mean time between the last administration of clopidogrel (h) Aspirin |
5 25 |
6 25 |
0.90 |
| Low-molecular-weight heparin | 20 | 22 | 0.94 |
| Hemoglobin (g/L) | 133 (111-139) | 132 (110-141) | 0.90 |
| Operative Data | |||
| Number of grafts | 3.1 (2.2-3.6) | 3.4 (3.0-4.1) | 0.89 |
| Saphenous vein | 3.4 (3.0-4.1) | 3.3 (2.7-3.7) | 0.87 |
| Left internal thoracic/radial artery | 1 (1.0) | 1 (1.0) | 1.0 |
| Surgery (minutes) | 121 (115-147) | 125 (130-152) | 0.88 |
aData presented as mean with 95%confidence intervals, or number.
In this study, we present the effects of ABC use on postoperative bleeding and re-exploration rate, the amount of blood transfusion requirement due to excessive haemorhagie in our 25 off-pump emergent CABG patients who administered a high dose clopidogrel and 300 mgr ASA prior to surgery.
Materials and Methods:
Informed consent has been signed by the patients. 50 consecutive CAD patients with unstable angina unsuitable for percutanous coronary intervention and scheduled for urgent or acute isolated CABG at our hospital were included after the ethics committee approval of the study. 600 mg clopidogrel and 300 mg aspirin have been administred orally in all patients prior to coronary angiography. The patients divided into two groups. 25 patients received 10 mL local ABC (SG), in the remaining patients placebo has been used locally (CG). Blood platelet counts, activated partial thromboplastine time (aPTT), International normalized ratio (INR), activated coagulation time (ACT), and bleeding time (BT) was measured, preoperatively. The patients with bleeding history, disorders of bleeding, chronic renal failure, chronic obstructive pulmonary disease have been exluded from the study. When we compared the patients’ charecteristics in both groups, there was no statistical differences. The preoperative charecteristics of the patients have been summarized in Table 1. The ICU team was not informed about the bleeding control method. The invitro effect of ABC in heparinised blood is demonstrated in Figs. (1, 2). After invitro ABC application, we collected the immediate cloths. We investigated microscopic examination of this cloths has also been demonstrated in Fig. (3). At the same time, in preoperative period, to show the clear effects of ABC solution on heparinised plasma and blood, we present Video 1.
Operative Technique:
We performed urgent beating heart CABG without the use of ECC in all 50 patients. In those patients, left internal thoracic artery, saphenous vein and the radial artery as conduits have been used. Totally 7500 IU intravenous heparin was given prior to harvesting of the conduits. We provided ACT level between 350-450 sec. for all patients. After median sternotomy incision, we performed distal anastomosis using intracoronary shunts and heart stabilisator. The proxymal anastomosis was made using an aortic side clamp. After surgery, protamine sulphate was administrated for neutralization of heparin. For bleeding control, an electrocautery and hemoclips were used. After the completion of CABG procedures, a 10 ml ABC has been sprayed over the mediastinum including over conduits including ITA, and epicardium via simple rapide ejection method using a syringe in SG (n=25) (Video 2). Very rapide protein network formation was clearly seen immediately after the use of ABC. Bleeding was easily controlled in every patient. Ankaferd has also been applicated to epicardial fat. The sternotomy incision has been re-approxymated using a surgical steel wire. Postoperative coagulation tests including ACT and INR, platelet counts, and aPTT was recorded for each patient every 8 hours during ICU follow-up, postoperatively. Hemoglobine and hematocrite values have also been examined. There was no any statistical difference when we compared hematocrite level, coagulation test results, and platelet counts. The amount of mediastinal bleeding, transfused PRBC and blood products have been compared in both groups. The decision to perform resternotomy was made by the surgeon on call and based on conventional guidelines: drainage of >500 ml in the first hour, total drainage of>800 ml. in the first 2 h, 900 ml in the first 3h, >1000 ml in the first 4 h or 1200 ml in the first 5 h; 2. sudden massive bleeding or cardiac tamponade. Postoperative measurements of bleeding from the mediastinum, the amount of PRBC transfusion, and a number of bypass grafts have been summarized in Table 3.

demonstrates that rapid coagulation of heparinised blood (ACT level was 650 sec.). Thrombus formation is constituted immediately after ABC injection.
Outcome measures
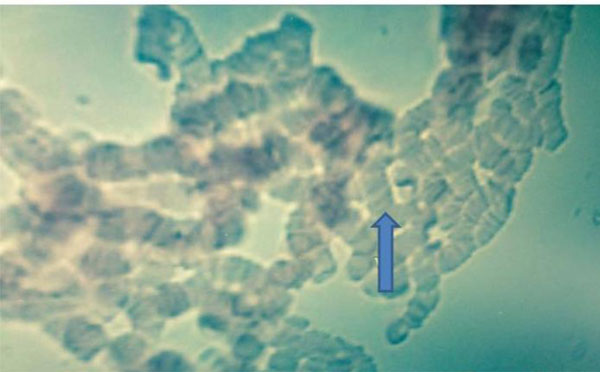
Microscopic examination of the cloth including eritrocyte aggregation after invitro ABC spraying.
Intraoperative blood loss was calculated by quantifying cell saver blood; postoperative bleeding (up to 24 h) was measured by mediastinal chest tube drainage following transfer to ICU. Excessive haemorrhage was defined as blood loss of >300 mL/h or >1000 mL/12 h, both within the first 24 h at ICU. Blood transfusion products (PRBC, fresh frozen plasma, platelet infusions) were used perioperatively at the discretion of anaesthetist and surgeon; indications for transfusion requirements were: haematocrit<25%, patients >75 years, haemodynamic instability, occurrence of tachycardia. Blood product use was documented during surgery, in the 24 h after arrival at ICU, and from 24 h until discharge. Indication for re-catheterization was an increasing creatine kinase-muscle-brain value of >2× the upper limit of normal, postoperative ST-segment elevations or adverse cardiac events.
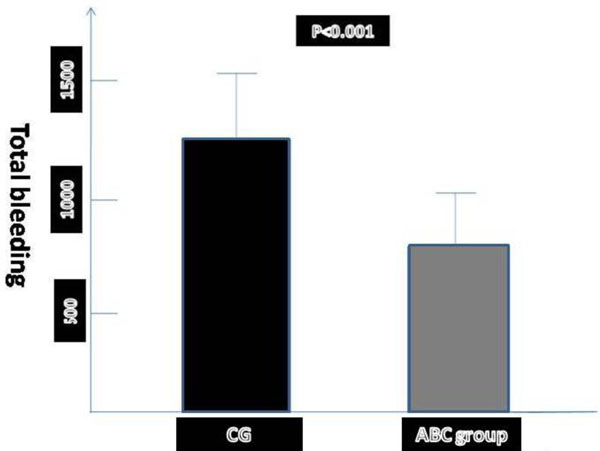
shows that the mean postoperative bleeding in off-pump CABG patients after randomization of treatment groups.
Statistical methods
| ABS Group (n =25) | Control Group (n =25) | P | |
|---|---|---|---|
| Early mortality | 0 | 0 | 1.0 |
| Reoperation(%)* | 0 | 4(16%) | 0.001 |
| Creatine kinase-MB, postoperative day 1 (μg/L) | 39 (29-54) | 24 (26-60) | 0.89 |
| Troponin-T, postoperative day 1 (μg/L) | 0.41 (0.22-0.45) | 0.50 (0.39-0.63) | 0.78 |
| Time to extubation (hours) | 7.2 (5.6-9.2) | 10.9 (7.9-13.1) | 0.002 |
| Hemoglobin at discharge (g/L) | 102 (86-119) | 108 (90-121) | 0.74 |
| Length of intensive care unit stay (hours)* | 26 (25-33) | 46 (29-56) | 0.0001 |
| Length of hospital stay (days)* | 4.8 (5.2-8.2) | 7.4 (5.0-9.3) | 0.0034 |
| Stroke | 0 | 0 | 1.0 |
| Q-wave infarction | 0 | 0 | 1.0 |
| Atrial fibrillation | 3 | 4 | 0.940 |
aData presented as mean with 95%confidence interval, or number.
| ABSG (n= 25) | CG (n=25) | P | |
|---|---|---|---|
| Bleeding (mL) | |||
| Operating room* | 230 (270-510) | 490 (470-580) | 0.001 |
| Intensive care unit* | 410 (360-540) | 680 (520-890) | 0.0022 |
| Total* | 530±280 | 990±440 | 0.001 |
| Autotransfusion (mL) | 210 (120-430) | 400 (280-620) | 0.001 |
| Transfusions (U), (Operating room) | |||
| PRBC* | 0.3 (0-0.9) | 0.8 (0.2-1.1) | 0.003 |
| Plasma* | 0 (0-0.2) | 0.7(0.4-1.6) | 0.36 |
| Plateletsb | 0.3 (0.2-0.6) | 1.2 (0.9-1.4) | 0.21 |
| Transfusions (U) (intensive care unit) | |||
| PRBC* | 0.3 (0-0.6) | 1.5 (0.3-2.6) | 0.03 |
| Plasma* | 0 | 0.5 (0-1.0) | 0.036 |
| Plateletsb | 0.1 (0-0.2) | 0.4 (0-0.7) | 0.021 |
| Transfusions (U), (total) | |||
| PRBC* | 0.7 (0.2-1.1) | 2.4 (1.1-4.1) | 0.001 |
| Plasma* | 0.1 (0-0.3) | 1.4 (0.5-2.2) | 0.004 |
| Plateletsb | 0.2 (0-0.4) | 1.9 (0.6-1.3) | 0.002 |
| Total blood products (U)* | 1.0 (0.1-2.1) | 3.9 (2.2-6.3) | 0.002 |
aData presented as mean and 95%confidence interval. bOne Unit is equal to 500 mL from 6 donors, PRBC = packed red blood cells.
Statistical analyses were performed using SPSS 15.0 software (SPSS Inc., Chicago, IL, USA). Comparison of treatment groups was drawn using Student's paired t-test, Mann–Whitney U, Kruskal–Wallis tests or chi-square analysis. Differences were considered significant for P<0.05. Follow-up evaluations were performed annually. All patients had been instructed to contact the hospital in the event of any unexpected deterioration of health. Long-term survival was estimated by standard Kaplan–Meier techniques; treatment was compared with log-rank analysis. Variables are reported as mean ± and 95%confidence interval (CI). The relationships between different treatment variables were assessed before and during regression analysis. We also used the propensity scores risk adjustment method to adjust baseline characteristics and/or clinical factors that could impact the decision to give patients clopidogrel and ASA.
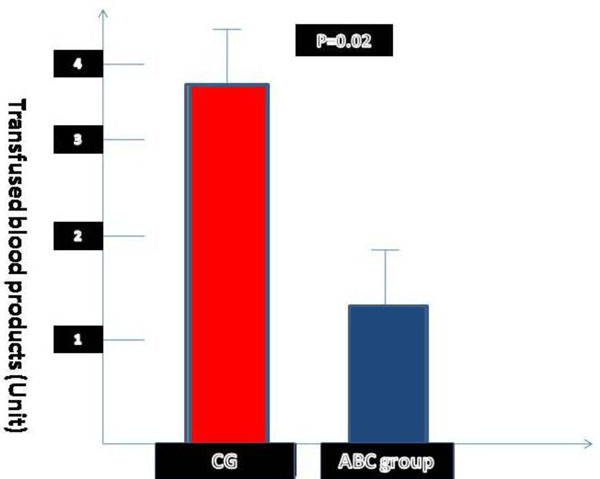
The amount of transfusions during hospital staying in patients who treated with ABS or saline (95%confidence interval).
Results
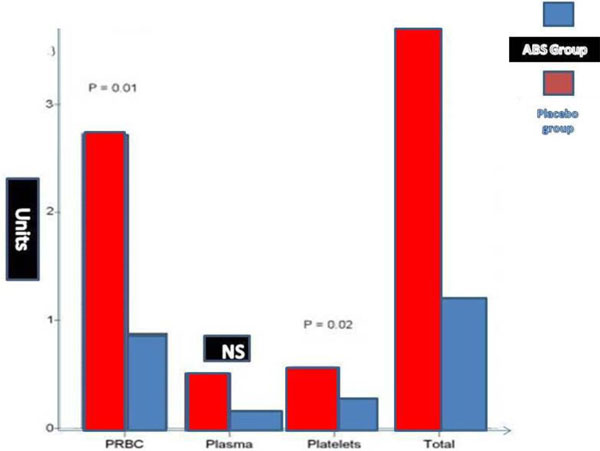
Transfusion of PRBC, plasma and platelets seperately during hospital staying in ABS and saline group (95%confidence interval).
There was no mortality in both groups. No re-operation was performed in ABC group. According to logistic EuroSCORE, there was no statistical significance in ABC and CG group (P=0.082). Duration of surgery and number of bypasses were similar between the groups but emergency surgery occurred twice as often in the CG. Four patients in ABC group and six patients in CG underwent percutaneous cardiac interventions within 6 month prior to operations.
The mean amount of bleeding after operation was 230ml in ABC group, and 490ml in CG (P=0.001). In ICU, bleeding from ABC and CG was 410ml and 680ml, respectively (P=0.0022). In ABC and CG group, total bleeding from the mediastinum was 530ml and 990ml, respectively (P=0.001). The amount of autotransfusion was as follows: 175ml in ABC group, and 290ml in CG (P=0.0031). No patient needed the surgical revision in ABC group, but four (16%) from CG group because excessive mediastinal hemorrahagie and cardiac tamponade. Seventeen patients from CG required blood transfusion due to low hematocrite level postoperatively. In CG, the mean hematocrite level was 17±2,3. Totally 12 patients in CG required PRBC transfusion in the early postoperative period. Transfusion of fresh frozen plasma and platelets in ABC group and CG were as follows: 0.2 and 0 in ABC group, and 0.3and 0.4 in CG. Total transfusion of PRBC in the operating room in ABC group and CG was 0.3 and 0.8, respectively (P=0.003). The mean transfused plasma and platelets in ABC group was 0 and 0.1; in CG these were 0.5 and 0.4 (P values of transfused plasma and platelets for ABC and CG were as follows: 0.36 and 0.21). Transfusions of PRBC in ICU for ABC and CG was 0.4 and 1.8, respectively (P=0.002). In ICU, the mean amount of transfused plasma was 0 and 0.5 in ABC and CG, respectively (P=0.0042). In ICU, the mean platelets transfusion was administered in ABC group 0.1 and in CG 0.4 U, respectively (P=0.021). A total transfusions of PRPC in the ICU in ABC group and in CG was 0.7 and 2.4 (P=0.001). Transfusion of total blood products in ABC group 1.1; and 3.9 in control group (P=0.001).
Postsurgery bleeding from mediastinum in different periods, and amount of transfusion are summarized in Table 3. No patient needed the surgical revision due to bleeding or cardiac tamponade in ABC group. Two patients (8%) from ABC group and 11 patients (40.1%) from CG needed blood transfusion after surgery (P=0,0001).
In the re-operations, in CG, there was no evidence of surgical reasons such as suture line or conduits’ branches. We used a low voltage electrocautery for exessive surrounding hemorrhagic area and we re-approxymated the sternum. In ABC group, the mean hematocrite level was 25±6,4 in the early postoperative period. In this patient group, blood products and/or PRBC has been administrated postoperatively in 7 patients (30.6%). In CG, the mean hematocrite level was recorded as 19±2,7 early after surgery. Total 14 patients (50.6%) received PRBC transfusion in the early postoperative period.
Discussion
A number of patients for emergent coronary artery bypass surgery due to peroperatuar PCI. Many of them are exposed to the platelet aggregation inhibitors such as high dose of clopidogrel and aspirin. The effects of antiag gregantion is continued 5 days following discontinuation. Therefore, the risk of severe bleeding complications are increased after surgery. As we know that a recent retrospective cardiac surgery data found an increased risk for transfusion and haemorrhagic complications in patients receiving clopidogrel within 24 h of surgery and suggested that delaying surgery by at least 24 h decreases this risk [11]. The use of off-pump instead of on-pump CABG attenuates perioperative bleeding and blood transfusion requirements [12, 13] but preoperative clopidogrel administration might diminish this effect. Higher rates of re-exploration for bleeding and a greater requirement for blood product transfusion in clopidogrel patients were observed after off-pump CABG surgery [14-16].
Major findings of our study have clearly showed that intraoperative local ABC transfusion requirements as a result of decreament of postoperative bleeding in off-pump CABG patients who treated with clopidogrel in addition to aspirin, <5 days prior to surgery. To the best of our knowledge, for the first time we evaluated the relationships between the post-surgery bleeding effects of ABC in our 25 off-pump CABG patients who medicated with high dose clopidogrel and ASA. This study also demonstrated that the relationships between the use of ABC and patients’ hospitalization and ICU staying time.
Ankaferd blood clotter is composed of a standardized mixture of the plants Thymus vulgaris, Glycyrrhiza glabra, Vitis vinifera, Alpinia officinarum, and Urtica dioica. All of those plants individually have some effects on the endothelium [6], blood cells [7], angiogenesis, cellular proliferation [8], vascular dynamics and mediators [9]. The basic mechanism of action for the haemostatic effects of ABC is currently unknown [19-22]. Experimental studies of ABC showed acute mucosal toxicity, hematotoxicity, hepatotoxicity, nephrotoxicity, and biochemical toxicity were not observed during the follow-up of the animal models and humans [24, 25]. But, three Ankaferd phase III studies showed it has decreased the bleeding from vascular port insertion, anterior epistaxis [20], and post-tonsillectomy hemorrhage [21]. Experimental studies have demonstraed the preclinical stage for the development of this hemostatic product [22, 23]. The hematological and biochemical safety of oral systemic administration of Ankaferd to rats pretreated using a warfarin have previously been reported by Cipil et al. [26].
Since individual clotting factors namely coagulation factor V, VII, VIII, IX, X, XI, XIII are not affected in the network formation, possible blood stopping process is driven based on protein agglutination. Erythrocytes and platelets were formed and gathered together to participate in the network formation. A hypothesis could be developed based on those observations that the network of ABC might cover the entire physiological haemostatic process without unequally affecting any individual clotting factor. Biochemical tests also revealed that total protein, albumin, and globulin levels significantly decreased with the interactions of ABC. Red blood cells come together to form vital erythrocyte mass blocks in the presence of ABC [27]. The network of ABC could cover the entire physiological haemostatic process without unequally disturbing individual clotting factors. According to the basic mechanism of action for ABC appears to be the formation of an encapsulated protein network for vital erythrocyte aggregation. We presented our experiences of local ABC solution use in emergent ACS in our urgent CABG administered preoperative high dose clopidogrel and aspirin preoperatively. As we know that interventional cardiologic approachs are frequently needed high dose clopidogrel and ASA [as irreversible or reversible antiplatelets] and/or anticoagulants. Clopidogrel and aspirin are affected platelet functions and increased the bleeding time in these particular particular patients. Therefore, we hypothesised that to decrease of re-exploration due to postsurgery cardiac tamponade due to mediastinal bleeding, blood and PRBC infusion; we decided that the use of local ABC solution in our 25 CABG operations, and we did not inform ICU personal about the application protocol for both groups. The mean hematocrit was lower in CG than in ABC group in the early period (P<0.05). No difference was detected between groups in routine coagulation measurements of INR, prothrombin time, or PTT at any time point. There was a >2-5 fold increase in blood product transfusions among patients in control group compared with ABC. The tables 2 and 3 describes the relationships between clopidogrel and ASA exposure, timing of transfusions, chest tube output and re-exploration rate. Patients exposed to clopidogrel and ASA were more likely to receive transfusions both in the intraoperative and postoperative periods. In addition, they were also more likely to have received a platelet transfusion intraoperatively. In the post-operative period, transfusion of platelets, PRBC, fresh frozen plasma were all used more frequently in the control group. Kalayci et al. have reported the intraabdominal hemostatic effect of ABC in an experimental liver injury in rat models [22]. They have suggested that the use of ABC shortened hemorrhagie from liver injury after organ injury. In another study, Cipil et collegues have showed that the amount of bleeding after ABC administration to amputed leg decreased by 53.8%in warfarin-treated group in animal models [26]. Previously published researchs demonstrated that ABC play an effective role of local hemostasis. The researchers offered as a therapeutic to provide local hemostasis control in clinical medicine. Ulus et al. have previously published the report that surgical and histopathological efficasy of topical ABC use for major arterial vessel injury [28]. They have found that the vessel lumens were enriched with erythrocyte aggregates followed ABC administration. They also showed that the other injured extremity vessels had no erythrocyte aggregation without the use of ABC solution [28].
Our study demonstrated that when we compared both groups chest tube output was greatest within 12 hours in CG. Multivariate analysis confirmed that CG patients received more blood transfusions and had more chest tube output when controlling all other factors. In ABC group, the mean amount of bleeding from the mediastinum was 230 mL and 410 mL 2. hour and 12. hour postsurgery, respectively. In ICU, bleeding from chest tube was lower in ABC group than from CG. In ABC group, total bleeding from the mediastinum was 530 mL. However, this value was 990 mL in CG. Therefore, the mean amount of autotransfusion was lower in ABC group. No patient required surgical revision due to bleeding or cardiac tamponade in ABC group. 4 patients from ABC group and Seventeen patients from CG needed blood transfusion after surgery. In the operations, there were no evidence of surgical reason which required suture or hemoclips in these patients.
Like an our study, Uzun et collegues demonstrated that successful application of ABC in 23 of the 25 bronchoscopic procedures in their patients for bronchial hemoptysis. This is the large case series demonstrated that endobronchial local application of ABC was effective in the management of bronchial bleeding due to local endobronchial malignant lesions [23]. Ozaslan et collegues showed the successful topical application of ABC in their 4 patient with gastric and duodenal variceal severe bleeding [24]. Beyazit et al. did report a success effect of ABC use in a case with lower gastrointestinal bleeding [25]. In addition, Kurt et al. have reported that the success topical use of ABC in their patient with gastrointestinal bleeding due to neoplasm [28]. The successful results of ABC use as a hemostatic agent in their 26 patients with bening lesion of gastrointestinal tracts has been reported by Kurt et collegues [29]. In this research, the authors have suggested the ABC as a primary treatment or as an adjuvant to conventional modalities used to control gastrointestinal bleeding. Bleeding sometimes cannot be controlled with current conventional methods, even during re-operations, when the focal surgical bleeding point cannot be found and bleeding is massive, originating from all of the surrounding tissues in CABG who treated with high dose of antiplatelets and anticoagulants. If urgent surgery is preferred after interventional approach, excessive bleeding induced by clopidogrel remains an issue. Blood transfusions during cardiac surgery are associated with increased in hospital morbidity [infectious complications] and mortality [30]. In this context, ABC may be of interest, because it reduces overall bleeding and transfusion requirements in patients exposed to aspirin.
Conclusion
Several nonrandomized studies have demonstrated that clopidogrel within 5 days of CABG is associated with increased blood loss, reoperation rates for bleeding, and increased use of blood products, including PRBC and platelets [30-33]. Guidelines recommend discontinuing clopidogrel for at least 5 days before elective CABG to limit chest tube out-put postoperatively and blood transfusions for at least 24 hours before CABG to reduce major bleeding complications. But, CABG surgery inevitable in some urgent situations. Our study shows that local use of ABC decrease the bleeding from the mediastinum after CABG. ABC seems to be effective agent to inhibit blood loss after CABG without any complication and provides a significant reduction of bleeding in patients medicated with high dose clopidogrel.
Study limitation
We described ABC use to control bleeding might fail to replicate the type of injury that would be likely to result in life-threatening bleeding in CABG patients, which should be considered a limitation of the present study. The histopathologic findings of the cloths suggest that ABC might affect global hemostasis by inducing a unique protein network formation, potentially representing a different mechanism of action among conventional antihemorrhagic drugs.


