All published articles of this journal are available on ScienceDirect.
Type of Valvular Heart Disease Requiring Surgery in the 21st Century: Mortality and Length-of-Stay Related to Surgery
Abstract
Aim:
While the incidence of rheumatic heart disease has declined dramatically over the last half-century, the number of valve surgeries has not changed. This study was undertaken to define the most common type of valvular heart disease requiring surgery today, and determine in-hospital surgical mortality and length-of-stay (LOS) for isolated aortic or mitral valve surgery in a United States tertiary-care hospital.
Methods:
Patients with valve surgery between January 2002 to June 2008 at The Ohio State University Medical Center were studied. Patients only with isolated aortic or mitral valve surgery were analyzed.
Results:
From 915 patients undergoing at least aortic or mitral valve surgery, the majority had concomitant cardiac proce-dures mostly coronary artery bypass grafting (CABG); only 340 patients had isolated aortic (n=204) or mitral (n=136) valve surgery. In-hospital surgical mortality for mitral regurgitation (n=119), aortic stenosis (n=151), aortic insufficiency (n=53) and mitral stenosis (n=17) was 2.5% (replacement 3.4%; repair 1.6%), 3.9%, 5.6% and 5.8%, respectively (p=NS). Median LOS for aortic insufficiency, aortic stenosis, mitral regurgitation, and mitral stenosis was 7, 8, 9 (replacement 11.5; repair 7) and 11 days, respectively (p<0.05 for group). In-hospital surgical mortality for single valve surgery plus CABG was 10.2% (p<0.005 compared to single valve surgery).
Conclusions:
Aortic stenosis and mitral regurgitation are the most common valvular lesions requiring surgery today. Surgery for isolated aortic or mitral valve disease has low in-hospital mortality with modest LOS. Concomitant CABG with valve surgery increases mortality substantially. Hospital analysis is needed to monitor quality and stimulate improvement among Institutions.
INTRODUCTION
Even though there has been a dramatic decrease in rheumatic heart disease over the last half century, there has not been a similar decline in the number of valve surgeries performed today [1-4]. This is mostly explained by a climb in calcific valve disease particularly aortic stenosis that is typically seen in the elderly, and in mitral valvular regurgitation related to floppy mitral valve/mitral valve prolapse [1,4-6]. These two valvular abnormalities will further increase as the population ages. Valvular heart disease often requires surgery particularly if severe and the patient is symptomatic [7]. Percutaneous valve replacement or repair are promising and may change the management of valvular heart disease in the future; however, typically valvular heart disease still remains a surgical disorder with substantial morbidity and mortality [8,9]. The vast majority of valve surgeries that are performed usually involve the aortic and/or mitral valves [5, 6, 10-12].
A wide range of in-hospital mortality associated with aortic or mitral valve surgery has been reported in the literature ranging from 1% to 8%; however, this in-hospital mortality reported does not reflect isolated valve surgery because coronary artery bypass grafting (CABG) or other surgical interventions are often included in the analyses [13-23]. In addition, in-hospital surgical mortality depends on patient age and co-morbidities, surgical volume for a particular hospital, and experience of the surgeons and health care team [23-25]. This retrospective study was conducted to define the most common type of valvular heart disease requiring surgery today, and determine the in-hospital surgical mortality and length-of-stay over a 6 year period (2002-2008) for isolated aortic or mitral valve surgery in the 21st century for a typical large tertiary-care Medical Center in the United States that serves a large referral base. The information gained can be used to compare future surgical outcomes as a means to determine progress and provide quality control not only for our Medical Center, but other major hospitals.
MATERIALS AND METHODOLOGY
Electronic medical records from The Ohio State University Medical Center (Columbus, Ohio, USA) from January 2002 to June 2008 were reviewed. The Ohio State University Institutional Review Board (IRB) approved this study; due to retrospective analysis, individual patient written informed consent was waived by the IRB. A total of 915 patients where identified who had open-heart surgery of at least the aortic or mitral valve. The majority of these patients at the time of their surgery also had an additional cardiothoracic procedure(s) including: multiple valve surgery (aortic, mitral, tricuspid and/or pulmonic), CABG and/or thoracic aorta surgery (Fig. 1). One hundred seventy patients and 15 patients had two and three valve surgery, respectively; 389 had concomitant CABG at the time of valve surgery with an average of 2.41 grafts per patient, and 101 had simultaneous thoracic aorta surgery at the time of their valve surgery. The remaining 340 patients who had isolated aortic or mitral valve surgery were further analyzed.
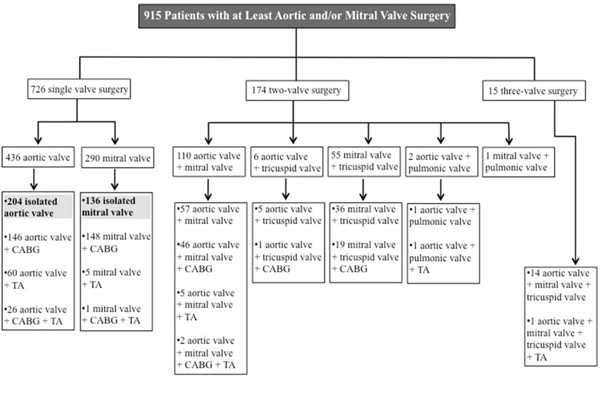
Patients with valvular heart disease and type of surgery performed at The Ohio State University Medical Center between January 2002 to June 2008 are shown. CABG=coronary artery bypass grafting surgery; TA=thoracic aorta surgery.
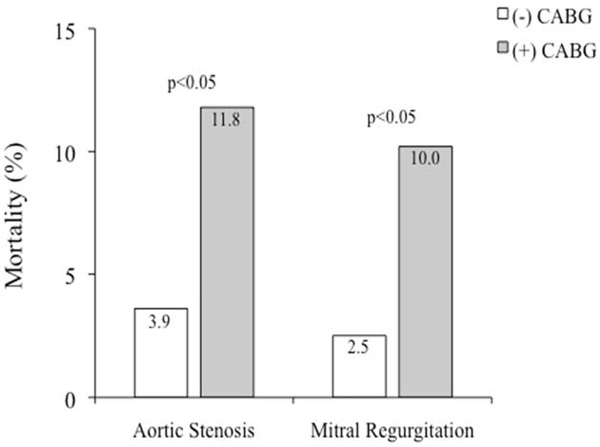
In-hospital surgical mortality for single valve surgery for aortic stenosis and mitral regurgitation with (+) or without (-) concomitant coronary artery bypass grafting (CABG) surgery is shown.
In-hospital surgical mortality and length-of-stay were determined. Patient hospital length-of-stay included only patients who survived hospitalization. Due to the wide range in hospital length-of-stay with potential outliers, median along with the mean values are presented.
Statistical Analysis
Descriptive data are shown as either mean ± standard deviation or as a median with a low and high range. To determine if there was a statistically significant difference in age among patient groups analysis of variance (ANOVA) was performed. To define if there was a statistically significant difference in the in-hospital surgical mortality and length-of-stay among patient groups a Fisher’s exac or Chi-square test was performed where appropriate. A p-value <0.05 was considered statistically significant.
RESULTS
The majority of patients who underwent valve surgery had other cardiac procedures or surgery in more than one valve (Fig. 1). In-hospital surgical mortality and length-of-stay that are presented only includes patients with isolated aortic or mitral valve surgery.
Aortic stenosis
There were 151 patients (89 male, 58.9%) who underwent isolated aortic valve surgery for aortic stenosis; 146 of these patients had aortic valve replacement and 5 aortic valve repair. The patients that underwent repair were not analyzed separately, but were included in the overall analysis for isolated valve surgery for aortic stenosis. The average age was 68.0 ± 13.2 years. The in-hospital surgical mortality was 3.9%. The mean hospital length-of-stay was 12.0 ± 11.2 days and the median hospital length-of-stay was 8 days ranging from 3 to 95 days.
Aortic Insufficiency
There were 53 patients (37 male, 69.8%) who underwent isolated aortic valve surgery for aortic insufficiency; 50 of these patients had aortic valve replacement while 3 aortic valve repair. The patients that underwent repair were not analyzed separately, but were included in the overall analysis for isolated valve surgery for aortic insufficiency. The average age was 50.2 ± 15.6 years. The in-hospital surgical mortality was 5.6%. The mean hospital length-of-stay was 16.2 ± 29.1 days and the median hospital length-of-stay was 7 days ranging from 3 to 155 days.
Mitral Stenosis
There were 17 patients (5 male, 29.4%) who underwent isolated mitral valve surgery for mitral stenosis; 16 of the patients had mitral valve replacement and 1 mitral valve repair in which these patients were analyzed together. The average age was 56.1 ± 13.3 years. The in-hospital surgical mortality was 5.8%. The mean hospital length-of-stay was 12.3 ± 7.0 days and the median hospital length-of-stay was 11 days ranging from 4 to 32 days.
Mitral Regurgitation
There were 119 patients (74 male, 62.1%) who underwent isolated mitral valve surgery for mitral regurgitation; 58 patients had mitral valve replacement and 61 mitral valve repair, and since the number of patients in each group was similar they were analyzed separately. The average age for the entire group was 56.3 ± 14.3 years. The in-hospital surgical mortality for the entire group was 2.5% (3.4% for replacement; 1.6% for repair). The mean hospital length-of-stay for the entire group was 12.7 ± 15.8 days (15.7 ± 17.5 days for replacement; 9.8 ± 13.0 days for repair) and the median hospital length-of-stay was 9 days ranging from 2 to 118 days (11.5 days ranging from 4 to 118 days for replacement; 7 days ranging from 2 to 98 days for repair).
There was a significant difference in age among the groups undergoing isolated valve surgery (p<0.0001). Patients with aortic stenosis where the oldest with a mean age of 68.0 ± 13.2 years compared to aortic insufficiency with a mean age of 50.2 ± 15.6 years (p<0.0001), mitral regurgitation with a mean age of 56.3 ± 14.3 years (p<0.0001), and mitral stenosis with a mean age of 56.1 ± 13.3 years (p<0.01). Patients with aortic insufficiency were the youngest compared to aortic stenosis (p<0.05) and mitral regurgitation (p<0.05). No significant difference in age was found between aortic insufficiency and mitral stenosis; this is probably related to the small number of patients in the mitral stenosis group. There was no significant difference in age between patients undergoing isolated valve surgery for mitral regurgitation and mitral stenosis.
There was no significant difference in-hospital surgical mortality among isolated valve surgery for aortic stenosis, aortic insufficiency, mitral stenosis, mitral regurgitation with mitral valve replacement, and mitral regurgitation with mitral valve repair (p=0.70; Table 1); however, there was a significant difference in median hospital length-of-stay among groups (p<0.05; Table 2). The median hospital length-of-stay was the shortest in patients who underwent surgery for aortic insufficiency and mitral valve repair for mitral regurgitation. The median length-of-stay was the longest in patients who underwent surgery for mitral stenosis and mitral valve replacement for mitral regurgitation.
In-Hospital Surgical Mortality for Isolated Valve Surgery for the Following Valvular Disorders
| Aortic Stenosis (n=151, 89 male) | Aortic Insufficiency (n=53, 37 male) | Mitral Stenosis (n=17, 5 male) | Mitral Regurgitation: Replacement (n=58, 29 male) | Mitral Regurgitation: Repair (n=61, 45 male) | |
|---|---|---|---|---|---|
| Mortality, n (%) | 6 (3.9) | 3 (5.6) | 1 (5.8) | 2 (3.4) | 1 (1.6) |
There is no significant difference among groups (p=0.70); n=patient number; %=percent of patients.
Hospital Length-of-stay (LOS) for Isolated Valve Surgery for the Following Valvular Disorders
| Aortic Stenosis (n=145) | Aortic Insufficiency (n=50) | Mitral Stenosis (n=16) | Mitral Regurgitation: Replacement (n=56) | Mitral Regurgitation: Repair (n=60) | |
|---|---|---|---|---|---|
| Mean LOS days | 12.0 ± 11.2 | 16.2 ± 29.1 | 12.3 ± 7.0 | 15.7 ± 17.5 | 9.8 ± 13.0 |
| Median LOS days (range) | 8 (3 to 95) | 7 (3 to 155) | 11 (4 to 32) | 11.5 (4 to 118) | 7 (2 to 98) |
| Median LOS ≤ 7 days, n (%) | 65 (44.8) | 28 (56.0) | 4 (25.0) | 17 (30.3) | 32 (53.3) |
| Median LOS ≥ 8 to ≤ 14 days, n (%) | 46 (31.7) | 11 (22.0) | 7 (43.7) | 20 (35.7) | 21 (35.0) |
| Median LOS > 14 days, n (%) | 34 (23.4) | 11 (22.0) | 5 (31.2) | 19 (33.9) | 7 (11.6) |
LOS includes only patients who survived hospitalization. There was a significant difference in LOS among groups (p<0.05); n=patient number; %=percent of patients.
There were 294 patients who had single valve surgery (aortic 146, mitral 148) and concomitant CABG surgery; the overall in-hospital surgical morality in these patients was greater compared to single valve surgery alone (10.2% versus 3.8%; p<0.005). In-hospital surgical morality for aortic stenosis and concomitant CABG surgery was greater compared to surgery for isolated aortic stenosis (11.8% versus 3.9%, p<0.05; Fig. 2). Likewise, in-hospital surgical morality for mitral regurgitation and concomitant CABG surgery was greater compared to surgery for isolated mitral regurgitation (10.0% versus 2.5%, p<0.05; Fig. 2).
DISCUSSION
Valvular heart disease is a progressive disorder, which often requires surgery when it is severe and/or the patient is symptomatic [7]. Over the last 50 years the incidence of rheumatic heart disease has declined, but the number of valve surgeries performed has not followed the decrease of rheumatic fever. This is mostly explained by an increase in the incidence of calcific aortic stenosis and mitral valve regurgitation due to floppy mitral valve/mitral valve prolapse in which usually is seen in the elderly [1-6]. As the population continues to grow in age, the number of valve surgeries will climb since both of these valve abnormalities deteriorate with age. The evolution of percutaneous valve replacement or repair perhaps will change the management of valvular heart disease in the future; however, typically valvular heart disease still remains a surgical disorder [8,9,11,12]. Thus, determining the outcomes associated with valve surgery is imperative in order to provide quality control, track progress and determine areas that require improvement in ones own Medical Institution. Moreover, the information gained can also serve as a guide to similar volume hospitals stimulating learning, progress and enhancement of patient care.
A wide range of in-hospital surgical mortality for aortic and mitral valve surgery has been reported ranging from 1% to 8% [13-24]. The mortality reported, however, does not reflect isolated valve surgery because patients during valve surgery often undergo additional surgical procedures including multiple valve surgery, CABG surgery, and aorta surgery to mention a few. Further, in-hospital surgical morality typically is less for mitral valve repair (between 1-2%) as compared to mitral valve replacement for mitral regurgitation [18-21]. Variations in hospital mortality are also related to several other factors including the overall clinical status of a patient, the number of valve surgeries performed in a particular hospital, and experience of the surgeon, anesthesiologist, intensive care personal, and other [23-25].
This study demonstrated that the majority of patients undergoing open-heart surgery have more procedures performed than just isolated valve surgery. As it was expected the number of patients that had surgery for mitral stenosis was small; this reflects the dramatic decrease of rheumatic fever in the last 50 years in the United States [1-4]. The most common valvular abnormality was aortic stenosis, which was followed by mitral regurgitation and then aortic insufficiency.
This study provides important information for morbidity and mortality related to valve surgery in a typical large tertiary-care Medical Center in the United States that serves a large referral base. The data shows that the in-hospital surgical mortality was relatively low for isolated aortic or mitral valve surgery ranging as low as 1.6% for mitral valve repair for mitral regurgitation and as high as 5.8% for mitral stenosis. Overall, there was no statistically significant difference in the in-hospital surgical mortality among groups, which may have been effected by the relatively low number of patients in the mitral stenosis group.
Patients who underwent isolated aortic valve surgery for aortic stenosis were approximately 12 years older compared to mitral stenosis and mitral regurgitation, and 18 years older compared to aortic insufficiency; despite increase in age in patients with aortic stenosis, there was no significant difference in the in-hospital surgical mortality. These findings are consistent with the pathophysiology of aortic stenosis in which removal of the fixed obstruction is associated with an immediate improvement in left ventricular performance and cardiovascular hemodynamic performance [6, 12]. Mitral valve repair was also shown to have a low in-hospital surgical mortality and short hospital length of stay, as been previously reported, mostly due to a less invasive procedure, favorable mitral valve anatomy, and patient selection [18-21].
It has been reported previously that surgical mortality associated with valve surgery increases when combined with CABG surgery [21, 22]. This study confirmed these findings demonstrating a significant increase in the in-hospital surgical mortality by approximately 2.5-fold when single valve surgery (aortic or mitral valve) was combined with CABG surgery. It is also known that the incidence of coronary artery disease is more common in patients with aortic stenosis as compared to the general population. This phenomenon most likely reflects similar pathogenetic mechanisms related to calcific aortic stenosis and atherosclerotic coronary artery disease [26-28]. As the population ages, coronary artery disease and aortic stenosis will more often be seen in the same patient; in order to keep surgical mortality low, as it is reported in this study, a hybrid approach of surgical replacement of the aortic valve and percutaneous coronary intervention may need to be considered in selected patients.
There are limitations related to this study. The etiology of valvular heart disease, which may affect in-hospital surgical mortality and length of stay, for isolated aortic or mitral valve surgery was not analyzed. Further, the patient population in our tertiary-care Medical Center may reflect a selection bias since most of these patients included complicated cases referred for advance management. Despite these limitations, the study does provide important information on morbidity and mortality related to overall isolated valve surgery with or without concomitant CABG surgery in a large tertiary-care Medical Center in the 21st century (i.e. in the real world), which is a strength of the study.
CONCLUSIONS
In summary, aortic stenosis and mitral regurgitation are the two most common causes of valve surgery today. The incidence of these valvular disorders will continue to increase as the population ages. Surgery for isolated aortic or mitral valve disease today has low in-hospital surgical mortality with modest hospital length-of-stay when performed in a large tertiary-care Medical Center. Concomitant CABG with valve surgery increases mortality substantially. Individual hospital analysis is strongly encouraged to provide “self-assessment” that can serve to provide quality control and means for improvement given that these procedures will continue to increase. Moreover, sharing of data and findings can stimulate learning, progress and improvement between Medical Institutions.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
FUNDING SOURCE
None
ACKNOWLEDGEMENTS
The authors would like to thank Mahmoud Abdel-Rasoul, MS, MPH, from the Center for Biostatistics at The Ohio State University, for his assistance in the statistical analysis.


