All published articles of this journal are available on ScienceDirect.
Patient with Hypertriglyceridemia, Type 2 Diabetes, and Chronic Kidney Disease Treated with Atorvastatin and Omega-3 Fatty Acid Ethyl Esters
Abstract
This is a case report that describes a 67-year-old woman with mixed hyperlipidemia and diabetic nephropathy. She was initially prescribed a combination of simvastatin plus gemfibrozil by her general practitioner (GP). When referred to our cardiovascular unit, we further diagnosed the patient to have mixed hyperlipidemia and rhabdomyolysis. Because of concerns with her chronic kidney disease (CKD), we temporarily stopped all her drug treatments and started insulin treatment for her type 2 diabetes (T2D). A month later when her T2D was stabilised, we prescribed atorvastatin and an omega-3 fatty acid ethyl ester supplement to treat her hypertriglyceridemia. Within two months her blood lipids were within the recommended range. In patients with stage 3–5 CKD, it is not advisable to prescribe the fibrate gemfibrozil, particularly in combination with a statin that is metabolised predominantly in the kidneys. To minimise adverse events without compromise on efficacy, we used a combination of omega-3 fatty acid ethyl esters, which are not metabolised in the kidneys, with a statin that is minimally metabolised in the kidneys for the treatment of her hyperlipidemia.
INTRODUCTION
We describe a 67-year-old woman with mixed hyperlipidemia and diabetic nephropathy. She was initially prescribed a combination of simvastatin plus gemfibrozil by her General Practitioner (GP) and was then referred to our unit with rhabdomyolysis (Table 1). Drugs were temporarily discontinued and she only received insulin. Current evidence suggests that statins can improve the glomerular filtration rate (GFR) or delay GFR decline in patients with type 2 diabetes (T2DM) [1]. However, the patient’s general practitioner had initially prescribed a combination of simvastatin plus gemfibrozil: both of these drugs are substantially metabolized by the kidneys. As the patient already had stage 3 chronic kidney disease (CKD; estimated glomerular filtration rate 30 - 59 ml/min/1.73m2), which is frequently seen in diabetic subjects [1, 2], this resulted in the accumulation of both drugs in the blood and she developed rhabdomyolysis. Rhabdomyolysis associated with the simvastatin + gemfibrozil combination, is an adverse effect seen even in patients with normal kidney function. To control the hyperlipidemia, we changed her treatment to an omega-3 fatty acid ethyl ester supplement (Omacor®) in combination with atorvastatin; both drugs have negligible renal metabolism [3-5].
Laboratory Measurements
| November 23, 2011 | February 21, 2012 | March 22, 2012 | May 16, 2012 | |
|---|---|---|---|---|
| CK (IU/L) | 145 | 3,250 | 157 | 133 |
| AST (IU/L) | 24 | 135 | 28 | 20 |
| ALT (IU/L) | 26 | 43 | 30 | 23 |
| LDH (IU/L) | NA | 1,485 | 312 | 253 |
| Glomerular filtration rate mL/min/1.73m2 | NA | 41 | 44 | 44 |
| Serum potassium (mmol/L) | 4.1 | 6.9 | 4.7 | 4.2 |
| Blood platelet count (/µL) | NA | 272,000 | 254,000 | 261,000 |
ALT = alanine aminotransferase; AST = aspartate aminotransferase; CK = creatine kinase; LDH = lactate dehydrogenase.
PATIENT HISTORY
A 67-year-old woman presented to her general practitioner on November 23, 2011. Five years previously, she had been diagnosed with T2DM, and was taking sitagliptin (100 mg/day). Her condition had now progressed to diabetic nephropathy with a reduced GFR of 41 mL/min/1.73m2. To help control her T2DM, she had been restricting her intake of carbohydrates and animal fat, with no restrictions on her dietary protein. She weighed 70 kg [body mass index (BMI) = 27.3 Kg/m2). Electrocardiography findings were normal, and the patient had no obvious symptoms or family history of cardiovascular disease (CVD). She was a non-smoker and did little physical activity. In addition to sitagliptin, hergeneral practitioner began treatment with simvastatin (40 mg/day) and gemfibrozil (1200 mg/day). She was also taking quinapril (20 mg/day) and aspirin (100 mg/day).
We first saw this patient in our hospital cardiovascular unit on February 21, 2012. In addition to T2DM and CKD, we diagnosed the patient had mixed hyperlipidemia (Fig. 1) and rhabdomyolysis (diffuse myalgia, low fever, fatigue, dark urine). Her heart rate was 92 bpm, while her left ventricular end-diastolic diameter (43 mm) and left ventricular ejection fraction (63%) were normal. Laboratory tests showed she had raised activities of serum creatine kinase (CK), aspartate aminotransferase (AST), and lactate dehydrogenase (LDH) (Table 1). Because of our concerns with her CKD, we temporarily discontinued all her drugs and started insulin treatment for her T2DM.
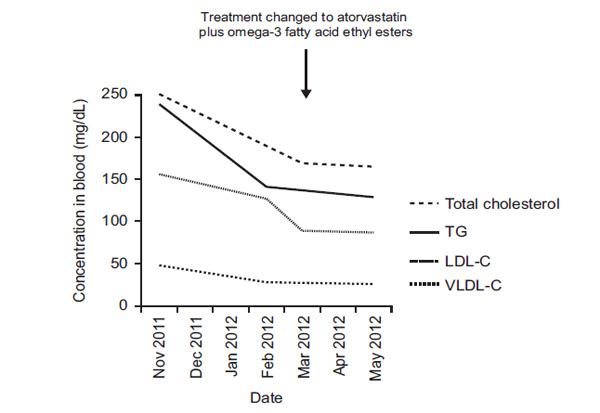
Fasting blood lipid levels throughout treatment.
A month later, her serum activities of CK, AST, and LDH were within the reference range (Table 1). We restarted sitagliptin (100 mg/day) and quinapril (20 mg/day), and changed her statin to atorvastatin (40 mg/day). We also prescribed an omega-3 fatty acid ethyl ester supplement (Omacor® 4 g/day, Abbott Laboratories (Hellas) SA, Athens, Greece) specifically to treat her hypertriglyceridemia. We also recommended lifestyle changes for the patient: she was started on the National Cholesterol Education Program Step II diet, which is reported to help lower blood total cholesterol and low-density lipoprotein cholesterol concentrations [6, 7], and she was set a goal of walking for 60 min at least 5 days/week.
By May 16, 2012 her blood lipids were within the recommended range according to our departmental guidelines (LDL-C <100 mg/dl and TGs <150 mg/dl – Fig. 1). She had lost 2 kg in weight (BMI 26.7 Kg/m2) since November 2011, her blood pressure had reduced from 140/80 to 125/75 mmHg, and her heart rate was now 78 bpm. After 2 months of treatment with atorvastatin and omega-3 fatty acid ethyl ester supplementation, her GFR was 44 mL/min/1.73m2. There were no side effects. As of June 2012, she has T2DM (HbA1c = 6.8%) and stage 3 CKD, with no abnormalities in her blood lipid profile. No additional treatments are currently planned.
DISCUSSION
This overweight patient with diabetic nephropathy developed rhabdomyolysis, presumably as a side effect of the simvastatin + gemfibrozil combination; the combination of simvastatin + sitagliptin might have also played a role [8]. Age and DM are also associated with statin-induced rhabdomyolysis and may have played a role in this case, however the simvastatin + gemfibrozil combination is the main suspect [9]. In patients with stage 3 - 5 CKD, it is not advisable to prescribe the fibrate gemfibrozil, particularly in combination with a statin such as simvastatin that is predominantly metabolized by the kidneys; this is a very high risk regimen [10].
Patients with stage 3 - 5 CKD make up a substantial proportion of high-risk patients with cardiovascular disease (30% of coronary heart disease patients and 20 - 40% of diabetic patients) [10-12]. Patients with both T2DM and CKD are at particularly high risk of cardiovascular disease [13-17] and it is imperative to monitor their GFR. This need is reinforced by the fact that diabetic patients have very frequently both hypertriglyceridemia and CKD and thus physicians should be aware of the recommended treatment in such patients [18]. The recommended treatment for patients with diabetic nephropathy is to reduce the risk or slow the progression of nephropathy and optimize glucose control [5, 18-23]. Where required, the treatment plan may need to be adjusted over time to reduce or manage adverse events. Data from post-hoc analyses of statin trials indicate a beneficial effect of statin therapy on cardiovascular disease outcomes in patients with stages 2 and 3 CKD; the benefit was particularly marked in patients with both CKD and diabetes [24-26]. A further complication of the disease management plan, most patients with stage 3 - 5 CKD also have mixed dyslipidemia [23, 24].
Our aim for this patient was firstly to control her T2DM [23], to protect her from the cardiorenal syndrome [21, 22] and then to reduce her blood lipid levels down to the guideline range [23]. A meta-analysis of 26 clinical trials involving over 25,000 patients showed that statins are effective in the treatment of dyslipidemia in non-dialysis patients with CKD [26]. Furthermore, the authors concluded that statins significantly reduced the risk of all-cause and cardiovascular mortality in this patient group.
Omega-3 fatty acid ethyl ester supplementation is an effective and well-tolerated treatment that can be combined with statins to further reduce blood triglyceride levels [27-30]. Recent European guidelines propose that the combination of omega-3 fatty acid ethyl esters, which are not metabolized in the kidneys, with a statin that is minimally metabolized in the kidneys (e.g. atorvastatin, fluvastatin) is effective and well tolerated in the treatment of mixed hyperlipidemia [23].
CONCLUSIONS
In combination with atorvastatin, an omega-3 fatty acid ethyl ester supplement was effective and well-tolerated treatment for this patient’s mixed dyslipidemia.
CONFLICT OF INTEREST
The author(s) confirm that this article content has no conflicts of interest.
ACKNOWLEDGMENTS AND FUNDING
The authors acknowledge the editorial assistance provided by Adelphi Communications Ltd, UK, which was supported by an unrestricted educational grant from Abbott Products Operations AG, Allschwil, Switzerland.
Writing assistance for this paper was supported by an unrestricted educational grant from Abbott Products Operations AG, Allschwil, Switzerland.


