All published articles of this journal are available on ScienceDirect.
Spontaneous Dissection of Right Coronary Artery Manifested with Acute Myocardial Infarction
Abstract
Spontaneous coronary artery dissection is a rare cause of acute ischemic coronary events and sudden cardiac death. It usually occurs in young women without traditional risk factors for coronary artery disease during pregnancy or postpartum period. However, it has also been reported in patients with atherosclerotic coronary disease. We present a case of spontaneous right coronary artery dissection in a 48-year male with recent myocardial infarction and previous percutaneous coronary intervention.
INTRODUCTION
Spontaneous coronary artery dissection (SCAD) is an infrequent event and an unusual cause of acute coronary syndrome with an estimated prevalence of 0.7‰ in a recent angiographic study [1]. It usually occurs in young women during pregnancy or postpartum period, and in most cases it involves a single coronary artery [2]. Multivessel SCAD is extremely rare and associated with high mortality rate [3]. Apart from pregnancy-related SCAD, vigorous exercise, sexual intercourse, isolated fibromuscular dysplasia, recent chest trauma, cocaine abuse, drugs such as cyclosporine, Marfan and Ehlers-Danlos syndromes, and some autoimmune diseases (Kawasaki, systemic lupus erythematosus and rheumatoid arthritis) have been associated with SCAD [3]. SCAD has also been reported in patients with atherosclerosis [4].
We describe a case of spontaneous right coronary artery (RCA) dissection in a 48-year male who had an inferior wall myocardial infarction (MI) 3 weeks before and had a percutaneous coronary angioplasty with stent implantation in a different segment of the RCA 5 years ago.
CASE
A 48-year-old man was referred to our hospital for coronary angiography due to a recent inferior wall MI for which he was initially treated with thrombolytic therapy. He had a history of coronary disease with a previous percutaneous coronary angioplasty in RCA (Fig. 1A, B) 5 years ago due to unstable angina. The patient had a history of hypertension and smoking (20 cigarettes per day). No history of collagen tissue disease, recent blunt chest trauma or use of cocaine and amphetamines was reported. Physical examination was unremarkable. The patient was on aspirin (100 mg od), clopidogrel (75 mg od) and metoprolol (50 mg twice daily).
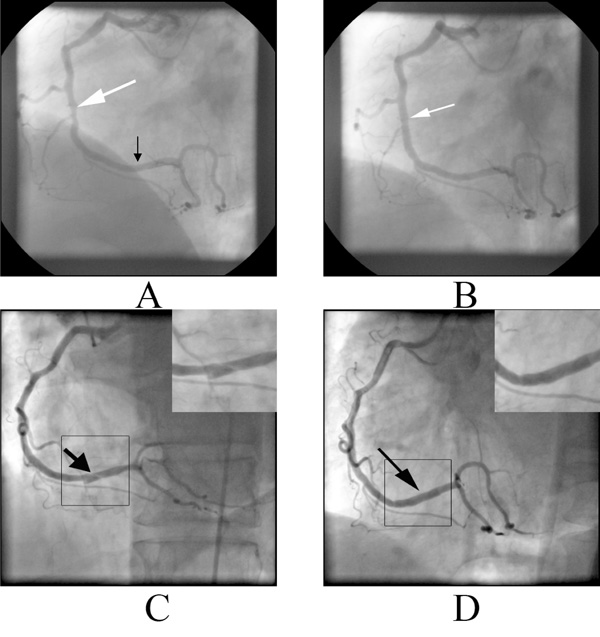
A. Coronary angiogram five years before showing the lesion in the middle RCA (white arrow). The distal RCA is normal, B. The artery after stenting of the lesion (white arrow), C. Spiral dissection in the distal RCA (black arrow) manifested with inferior acute myocardial infarction. The dissection is also depicted in magnification on the upper right corner, D. Distal RCA after stenting of the dissection (black arrow). The restoration of vessel patency after successful stenting is also depicted in magnification on the upper right corner.
The electrocardiogram showed inverted T waves in the inferior leads II, III, aVF. The laboratory studies were normal. Coronary angiography revealed normal left main coronary artery, left anterior descending and circumflex artery. The RCA had a spiral dissection distally, whereas the stent proximally was patent without evidence of neointimal hyperplasia (Fig. 1C). Ventriculography showed mild hypokinesia of inferior wall with an ejection fraction of 50%.
The spontaneous RCA dissection was treated with percutaneous coronary angioplasty and drug eluting stent implantation, which successfully covered the dissection (Fig. 1D).
DISCUSSION
As opposed to iatrogenic coronary dissection during percutaneous coronary angioplasty, spontaneous dissection is an extremely rare clinical condition [1]. SCAD usually affects young women though it is well described in males and the elderly [1]. Left anterior descending artery is the most common site of dissection, but involvement of the left main coronary artery, left circumflex artery and RCA may also occur [5]. RCA is the most commonly involved vessel in men [5].
The clinical manifestation of SCAD ranges from asymptomatic to acute coronary syndrome, cardiogenic shock and sudden cardiac death [6]. The number of involving arteries, the rate of propagation of the dissection, and the extent of involvement also affect the clinical manifestations [4]. In our case the patient presented with MI.
Pathophysiologically, non-atherosclerotic SCAD originate from a hematoma in the outer third of the media. When present, an intimal tear may decompress the hematoma in the false lumen and protect against vessel occlusion [7]. In about 30% of SCAD cases the underlying cause is an atherosclerotic plaque rupture [8]. Coronary dissections in atherosclerotic patients tend to occur in advanced ages, more often in men and usually affect the RCA as in our case [8]. The increased density of vasa vasorum and the elevated shear stress are precipitating factors that may lead to rupture of the intima, thereby creating a subintimal hematoma and finally leading to a dissection [7]. In our case it is most likely that the dissection developed in a normal, non-atherosclerotic, coronary region given that this area was visualized normal in the coronary angiogram 5 years earlier. However, one could not exclude the development of atherosclerosis in that region in the ensuing 5 years and subsequent dissection.
Coronary angiography confirms the diagnosis of SCAD in most of the cases; however, using angiography alone, the true incidence of SCAD is likely underestimated [5]. Intravascular ultrasound is a complementary technique that can be used in the identification and assessment of coronary dissection. Intravascular ultrasound can distinguish atherosclerotic stenosis from intramural hematoma, and also detect the medial dissection, false lumen, true lumen, and if present, the intimal flap [9]. Multidetector computed tomography coronary angiography has also been used in the detection and mainly in the follow up of SCAD [10].
Although various therapeutics strategies have been proposed, optimal treatment of SCAD is still unclear. Medical treatment can be considered in asymptomatic patients and in the cases of distal dissection or preserved coronary flow [11]. The role of thrombolytic therapy is controversial. It is a reasonable therapeutic approach for SCAD patients with acute MI treated in centers without coronary angiography facilities as in our patient [12]. However, thrombolytic therapy has been associated with the extension of dissection due to increased bleeding in the vessel wall [13] and hemorrhage of the vasa vasorum with bloody effusions inside the vessel wall, causing compression of the true lumen, further lumen reduction, and extension of the dissected area [13]. Therefore, thrombolytic treatment should be delayed until coronary angiography is performed. Percutaneous coronary intervention is the first therapeutic choice in single vessel dissection with persistent impairment of blood flow and ongoing symptoms of ischemia. Balloon dilatation without stenting should be avoided, whereas coronary stenting has been used successfully in selected cases where the true and false lumens were clearly distinguishable and the dissection flap did not involve a long segment [14]. Finally, coronary artery bypass is the treatment of choice in the cases with left main stem involvement, multiple vessel disease, ongoing ischemia refractory to medical or interventional treatment and hemodynamic instability [15].
CONCLUSION
In conclusion, SCAD is a rare cause of acute coronary syndromes. It should always be suspected as cause of acute coronary syndromes in young female patients, especially during pregnancy. Although in most of the cases SCAD affects non-atherosclerotic vessels cases have been reported in patients with coronary artery disease. In our case a patient with known coronary artery disease presented with a acute MI due to SCAD and was successfully treated with stenting of the affected segment of RCA.


