All published articles of this journal are available on ScienceDirect.
Combined Endovascular/Surgical Management of a Ruptured Para-Anastomotic Aneurysm of the Left Common Iliac Artery#
Abstract
A 75-year old man presented with signs and symptoms of acute abdomen and a clinical picture of hypovolemic shock. An emergency CT scan revealed a ruptured para-anastomotic left common iliac artery aneurysm. The patient had undergone an elective abdominal aortic aneurysm repair operation and placement of an aortoiliac bifurcated graft 10 years before. Para-anastomotic aneurysms had developed in all 3 (aortic and the 2 iliac) anastomosis. As the patient was highrisk, a combined endovascular/surgical approach was undertaken. The patient was discharged 4 days later.
This article discusses the applicability of endovascular procedures in emergency settings to high-risk patients.
INTRODUCTION
Ruptured abdominal aortic aneurysms (rAAAs) have mortality rates as high as 90%; about half of the patients die before reaching the hospital [1]. The surgical repair of rAAAs has a perioperative mortality of up to 70% [2]. Compared with open repair, endovascular aneurysm repair (EVAR) is associated with lower perioperative (as well as long-term) mortality rates [3]. A recent retrospective study reviewing a single centre’s 10-year experience with emergency EVAR for ruptured abdominal aortoiliac aneurysms showed a 30-day mortality rate as low as 13% [4]. It has been supported that “EVAR should be the gold standard for rAAAs” [5].
We present a high-risk patient with a ruptured para-anastomotic iliac artery aneurysm treated successfully with a combined endovascular and surgical approach.
CASE REPORT
A 75-year old man arrived at the Emergency Department of our Hospital with signs and symptoms of acute abdomen and a clinical picture of hypovolemic shock. His physical examination revealed a tender pulsatile mass in the lower abdomen. The following vital signs were recorded: blood pressure: 90/65 mmHg; heart rate: >100 beats/min; temperature: 37.0 °C. The patient had a hematocrit of 26.5 and a haemoglobin concentration of 8.4 g/dl.
His past medical history included an elective open abdominal aortic aneurysm repair operation with employment of an aortoiliac bifurcated bypass graft 10 years ago. A follow-up CT examination 2 years later had showed the development of para-anastomotic aneurysms in all 3 (the aortic and the 2 iliac) anastomoses. The patient suffered from chronic obstructive pulmonary disease and arterial hypertension. He had suffered an acute myocardial infarction in 2006 for which he had undergone a 3-vessel coronary artery bypass graft operation. Furthermore, he was suffering from moderate to severe cardiac insufficiency (ejection fraction: 30%). As he was a high-risk individual, it was decided that a conservative approach should be undertaken for the 3 para-anastomotic aneurysms; an annual CT scan was performed at another center to evaluate their enlargement.
An emergency abdominal CT scan revealed a rupture of the left common iliac artery aneurysm (Fig. 1a). A digital subtraction angiography verified the diagnosis (Fig. 1b).
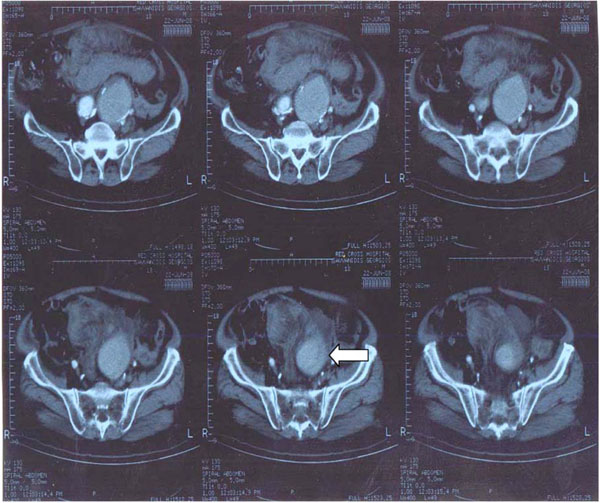
A CT scan showing the ruptured left iliacpara-anastomotic aneurysm (arrow).
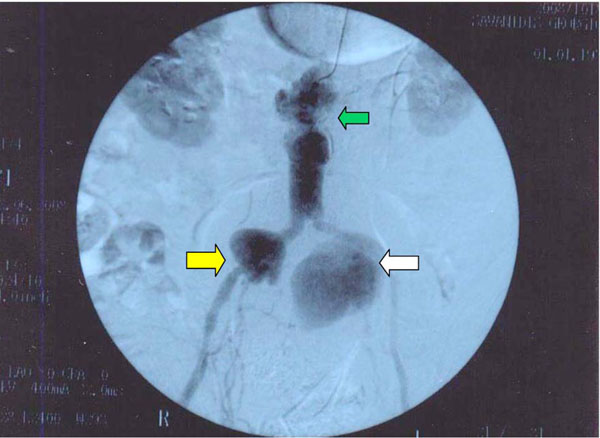
Digital subtraction angiography showing the ruptured left common iliac para-anastomotic aneurysm (white arrow), as well as the right common iliac (yellow arrow) and aortic (green arrow) para-anastomotic aneurysms.
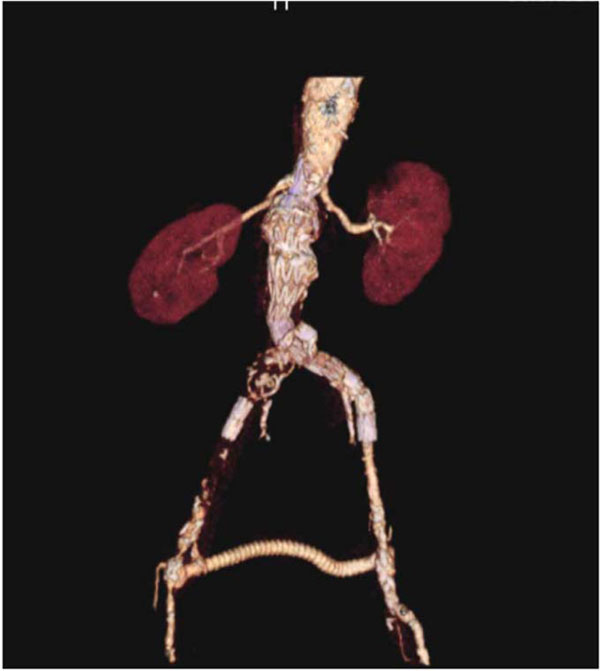
3-D digital computed aortography 3 months following the procedure.

3-D digital magnetic aortography 3 months following the procedure.
Due to the patient’s severe co-morbidities, a combined endovascular/surgical approach was adopted. By use of a Merate 9-inch C-arm in the operating theatre, an aorto-uni-iliac Cook Zenith® endovascular graft 36-121 mm (Cook Medical, Bloomington, IN, USA) was employed on the left side to seal the ruptured aneurysm. A second Cook Zenith® endovascular graft 12-105 mm (Cook Medical, Bloomington, IN, USA) was added as an extension. On the contralateral side, a 14-mm plug was inserted in the right external iliac artery. Finally a traditional open surgical femoral-femoral bypass was performed by use of a GORE polytetrafluoroethylene 8 mm ringed graft (Gore Medical Products, Flagstaff, AR, USA) to provide blood supply to the contralateral limb.
During the procedure, both internal iliac arteries were spared. The total amount of radio-opaque material used was approximately 90 mm. The pre- and post-operative blood cultures did not reveal any micro-organism which could be held responsible for the development of the 3 para-anastomotic aneurysms.
The patient was hemodynamically stable during the procedure. The post-operative clinical course was excellent; the patient did not suffer from buttock claudication. He was released 4 days post-procedurally. A 3-D digital computed and magnetic aortography performed 3 months later revealed an excellent post-procedural outcome with no endoleaks (Figs. 2a & 2b).
DISCUSSION
By adopting a combined endovascular/surgical procedure, both the ruptured and the 2 other para-anastomotic aneurysms were successfully managed. Furthermore, as the patient was high-risk, the complications of a traditional open surgical procedure were avoided. The advantages of the endovascular approach for the management of the ruptured left common iliac artery aneurysm included avoidance of extensive blood loss, avoidance of compromising the hemodynamic stability and a fast and painless recovery.
The adoption of EVAR for rAAAs decreases periprocedural mortality compared with open surgical repair. A recent survival analysis comparing the results of EVAR vs. open surgical repair for rAAAs in a patient cohort of 43,033 Medicare beneficiaries suffering a rAAA matched by propensity score showed a benefit of EVAR over open surgical repair (P=0.0042) [3]. This advantage is extremely important, especially when considering the fact that most patients with AAAs are high-risk individuals. The considerable advantages that are coupled with EVAR (namely decreased mortality/morbidity rates and decreased hospital stay) render endovascular approaches more preferable when compared with open surgical repair operations [3-5].
In conclusion, our case lends support to the opinion that EVAR should be the treatment-of-choice for ruptured aneurysms if the appropriate conditions are feasible [4, 5]. The numerous advantages of this less invasive procedure may render EVAR the treatment-of-choice for the management of ruptured arterial aneurysms.


