All published articles of this journal are available on ScienceDirect.
Feasibility of Telephone-Based Cardiology Consultation: Comparison of Resource Use and Outcomes vs In-Person Consultation
Abstract
Introduction:
The COVID-19 (Coronavirus infectious disease 2019) pandemic has highlighted the need for alternative modalities to connect with outpatients beyond in-person clinic visits. In the present study, we evaluated the feasibility of a telephone-based teleconsultation cardiology service and compared the use of testing and outcomes between teleconsultation and traditional in-office consultations
Methods:
The study took place prior to the COVID-19 pandemic July 2019 to March 2020. Consult lists were reviewed by a cardiologist for patients appropriate for teleconsultation. Those patients were contacted directly and, if agreeable, a consultation was completed and any required testing was arranged. A series of patients seen in the clinic, matched for a reason for consultation and consulting a cardiologist, were compared in terms of testing frequency and outcomes.
Results:
Of 157 patients who felt appropriate for teleconsultation, 100 (63.7%) were successfully contacted and a teleconsultation was completed. Comparing patients undergoing teleconsultation with a matched series of patients seen in person in the clinic, there were no significant differences in testing utilization or outcomes, including emergency room or hospital admission within 30 days of consultation or death or adverse cardiac events at six months following consultation.
Conclusion:
Telemedicine can be successfully utilized as an alternative to traditional clinic consultation for selected patients needing cardiology consultation. This consultative modality does not appear to lead to utilization of increased testing or decreased quality or patient outcomes. Larger studies are needed to assess this mode of consultation.
1. INTRODUCTION
COVID-19 (Coronavirus infectious disease 2019) pandemic has highlighted the need to connect with patients outside of face-to-face visits [1, 2]. Telemedicine is an obvious solution and cardiologists have rapidly established telemedicine services to address this crisis [3]. The subspecialty of cardiology has previously focused on the utility of telemedicine for specific clinical problems, such as management of chronic heart failure and pre-hospital assessment of possible acute myocardial infarction. However, the use of telemedicine for routine outpatient cardiology consultative purposes is supported by limited experience and data [4, 5].
In the present study, we report the outcomes following the initiation of a telephone-based telecardiology consultation service and compare this service to in-person cardiology consultation. Importantly, this study took place prior to the beginning of the COVID-19 pandemic and thus was an assessment of patient and provider use of telephone-based consultation during a time when there were no impediments to a traditional in-person consultation. Our goal was to assess the performance of this service and measure utilization of testing and patient outcome compared with a traditional face-to-face evaluation.
2. METHODS
The study ran from July 2019 until the start of the COVID-19 pandemic in March 2020. In July 2019, we launched a unique phone-based telecardiology consultation program aimed at identifying cardiology consultations that could be managed via a “virtual” telephone-based platform. General cardiologists of the Pearsall Heart Hospital of the Geisinger Health System were assigned to this program on a rotating basis. The cardiologist reviewed the daily consultation requests and identified those appropriate for telephone-based consultation from the daily list of all consultations, including those requested as both “routine” and “urgent.” Requests that were deemed as not appropriate for telecardiology were referred to the standard in-person clinic. Specific criteria for “appropriate” patients were not defined, rather a consideration of a patient for the program was based on the cardiologist’s review of the reason for consultation and the patient’s medical record. The only absolute exclusions for patient inclusion were the inability of the patient to participate in a phone-based interaction due to lack of a dedicated private phone line or physical impediments (i.e., hearing impairment) and language barriers that required an interpreter.
Patients identified as appropriate for telecardiology were contacted by telephone by the cardiologist and offered this service. The patient’s consent to a telecardiology visit as well as their chief complaint, history, review of systems, and prior data were documented in the teleconsultation note. If the patient was not reached by phone after 2 attempts, they were referred to the central system scheduling service for further attempts at scheduling a standard clinic appointment. Because this was a pilot project to assess the feasibility of telephone-based new patient consults and billing codes for this type of encounter were not established at the time of the project, the initial telemedicine encounters were billed as “no charge” encounters. Data collected included the reason for consultation, the physician’s decision regarding appropriateness for a telephone consult, and any testing that was felt necessary. In addition, the following outcomes were collected from the medical record: 1) need for in-person cardiology follow-up within 30 days, 2) cardiovascular-related emergency visits or admissions within 30 days, and, 3) adverse cardiovascular outcomes within 6 months.
To compare teleconsultation test utilization and outcomes with those of standard in-office face-to-face consultation, a randomly chosen sample of standard face-to-face consultations, matched 1:1 to each teleconsultation for diagnosis and performing cardiologist, were assessed in an identical manner for resource utilization and outcomes. These visits were identified from among clinic consultations during the same period as the teleconsultation program.
2.1. Statistical Analysis
Statistical analysis was performed using Sigmastat v.4.0 software (Systat, San Jose, CA, USA). Comparisons of testing use and outcomes between teleconsultation and office consultation were performed using chi-square analysis of proportions. For all comparisons a 2-sided p<0.05 was considered significant.
3. RESULTS
The pilot study took place on 50 weekdays between July 17, 2019 and March 10, 2020. During that period, a total of 341 consult requests were reviewed by a teleconsultation cardiologist. Of these, 157 (46.0%) were deemed appropriate for telecardiology based on the cardiologist’s assessment of the clinical question and a review of the patient’s medical record. Of patients who felt eligible for a telecardiology consult, 100 teleconsultations were completed (63.7% of patients felt that this mode of consultation was appropriate). Fig. (1) summarizes patient eligibility and reasons for non-completion of teleconsultation among eligible patients. Only 9 patients (5.7%) who were deemed appropriate for a telecardiology consult were deferred due to patient refusal. The most common reason for failure to complete a teleconsultation was the failure to connect with the patient by phone (24.8%).
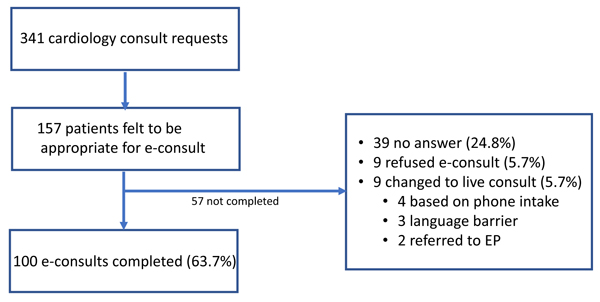
Table 1 summarizes the 10 most frequent diagnoses managed via telecardiology. The top 3 reasons for consultation which were completed via the teleconsultation process were chest pain, abnormal ECG, and palpitations. In total, there were 17 unique reasons for cardiology consultation which were addressed via teleconsultation.
Table 1.
| Reason for Consultation | Completed Teleconsultations |
| 1. Chest pain | 17 |
| 2. Abnormal electrocardiogram | 14 |
| 3. Palpitations | 10 |
| 4. Preoperative evaluation | 9 |
| 5. Congestive heart failure | 8 |
| 6. Tachycardia | 6 |
| 7. Valvular heart disease | 6 |
| 8. Premature ventricular contractions | 5 |
| 9. Abnormal echocardiogram | 5 |
| 10. Atrial fibrillation | 4 |
The breakdown of diagnoses in Table 1 was matched for the random review of in-person clinic consultations. Utilization of outpatient testing and outcomes comparing teleconsultations vs clinic consultations matched for a reason for consultation are summarized in Table 2. There were no significant differences between rates of overall testing or use of individual tests between tele- and in-office consults. There were no significant differences between emergency room visits or admissions at 30 days, and there were no deaths or adverse cardiac outcomes in either group in the 6 months following consultation.
| Teleconsultations | Clinic Consultations | p | |
|
Total Consultations Testing |
n 100 |
n 100 |
|
| Echocardiography | 21 | 34 | 0.057 |
| Stress testing | 24 | 25 | 1.000 |
| Cardiac CT | 6 | 5 | 1.000 |
| Holter/event monitor | 19 | 25 | 0.393 |
| Cardiac catheterization | 2 | 2 | 0.615 |
| Any testing | 60 | 71 | 0.137 |
| Outcomes | - | - | - |
| ER visit within 30 days | 10 | 4 | 0.166 |
| Admission within 30 days | 5 | 6 | 1.000 |
| Death/cardiac event within 6 months | 0 | 0 | n/a |
4. DISCUSSION
There is minimal data available evaluating the application of telemedicine to a general cardiology outpatient cardiology practice. The most robust data in telecardiology has focused telemonitoring of heart failure patients. These studies have generally suggested at most a modest benefit, with several large studies showing a lack of improvement in mortality and hospitalizations with the use of telemonitoring [4, 6]. While this lack of positive outcomes may be due to several factors, including the chronicity and progressive nature of heart failure, the COVID-19 pandemic has necessitated a re-examination of how telemedicine can be applied to all aspects of cardiology.
The present study examines the feasibility of performing initial cardiology consultation via selection of patients for telephone-only telemedicine. We were able to successfully complete teleconsultations across several cardiology diagnoses. Compared with diagnosis- and provider-matched in-person consultations, teleconsultations proved to be safe and cost-effective with regard to the use of downstream testing and resources. There were no differences in the use of cardiac testing between patients seen face-to-face and those assessed via telecardiology consultation. Even more important, there were no adverse cardiac events or cardiac-related deaths in either group in the 6-month period following consultation. Overall, these preliminary data support telemedicine as a viable platform for the performance of initial cardiology consultation in a significant proportion of patients. Despite the fact that teleconsultation was a new option for our patients, <10% failed to complete a teleconsultation due to refusal to participate. Given the robust uptake of telemedicine services and rapid achievement of a level of comfort with this modality among both providers and patients, it is likely that if our study was repeated during the COVID-19 pandemic, there would be an even higher acceptance rate and a higher percentage of consults considered appropriate for telecardiology.
The most common reason for failure to complete a consult in a patient deemed eligible for telecardiology was the inability to reach patients during working hours. This was mostly due to a shortcoming in the methodology of our program, specifically that our provider was initiating the teleconsultation without a previously scheduled consultation appointment time. It is likely that the use of a scheduling service to pre-arrange a consultation time would greatly decrease this failure rate.
It is notable that our study utilized a telephone-only telemedicine platform with acceptable results. The development of provider- and patient-friendly video platforms will likely improve this process [7]. As of March 2020, both video- and telephone-only telecardiology consultation have reimbursement codes put forth by the Centers for Medicare and Medicaid Services, further advancing both modalities as viable options for cardiology consultation services. There is limited data available regarding the differences in outcomes and quality of care when comparing telephone vs more advanced technology platforms, such as video or app-based telemedicine [8, 9]. Accumulation of experience in these more advanced technology platforms will likely reveal the optimal platform for telecardiology delivery.
The results of our study demonstrate the viability of telecardiology as a consultative modality even outside of the unique barriers to in-person evaluations caused by the COVID-19 pandemic. A recent report from Italy evaluated the outcomes associated with a mandated telecardiology consultation service initiated at the height of the COVID-19 pandemic [10]. That study reported that compared with historical in-person consultations, those patients managed via telemedicine were less likely to visit the emergency room for a cardiovascular cause during the follow-up period. While this may be interpreted as a positive quality marker associated with the telemedicine program, it should be noted that in this study, the telecardiology program was instituted during the height of COVID-19 pandemic, while the in-person clinic comparison was obtained from a pre-pandemic time period. Therefore, there is possible avoidance of the hospital setting due to fear of infection rather than as a result of the mode of cardiology evaluation was the reason for the findings. In contrast, both sections of our study took place prior to the onset of the COVID-19 pandemic in the United States, and therefore compared telemedicine vs in-person clinic visits during a time period in which patients did not have strong incentives to avoid an emergency or routine hospital visit. In this setting, we found no difference in emergency visits or admissions during the follow-up period. We interpret this finding as evidence that teleconsultation does not lead to increased downstream urgent evaluations. Admittedly, an alternative explanation could be that while we chose matched diagnoses for this comparative analysis, it is possible that the teleconsultation physician was biased to select patients that were perceived to be at lower risk given the lack of opportunity to evaluate these patients in person.
Our study suffers from obvious limitations in addition to those noted previously. Our sample size was limited and follow-up was short. The lack of randomization of patients to telemedicine vs live consultation limits the ability to assess application of teleconsultation to a general cardiology population.
CONCLUSION
The COVID-19 pandemic has forced cardiologists to accept telecardiology to assure continued access for patients during a time of great concern around social distancing and avoidance of contact with ill persons. Telecardiology is an ideal modality to maintain access for patients, including the elderly and those with significant comorbidities which make up a large segment of the cardiology patient community. It is likely that telemedicine will play an ever-expanding role in future medical care, and cardiology will be included in the growth of this modality. Evolving video technology and remote monitoring systems for blood pressure and telemetry will likely play a role in this growth. Future studies should evaluate the patient experience and patient satisfaction of teleconsultation vs in-person consultation. The acceptance of telemedicine as a cardiology subspecialty will undoubtedly lead to growth in virtual cardiology services beyond the COVID-19 pandemic.
ETHICS STATEMENT
This study was exempt given it did not involve patient contact or use of confidential records.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


