All published articles of this journal are available on ScienceDirect.
Prevalence of Major Cardiovascular Risk Factors and Coronary Heart Disease in a Sample of Greek Adults: The Saronikos Study
Abstract
Background:
Comprehensive data regarding prevalence of coronary heart disease (CHD) and associated factors in different geographical regions are very important to our understanding of global distribution and evolution of CHD. The aim of this study was to assess the current prevalence of self-reported risk factors and CHD in Greek adult population.
Methods:
A community-based cross-sectional study was conducted in May 2014, during an election day, among residents of Saronikos municipality (Attica region). Data were collected from face-to-face interviews. The study sample included 2636 subjects (men, 49.5%; mean age, 50.5; range 20-95 years), with similar age and sex distribution to the target population.
Results:
The age-standardized prevalence rates of five major risk factors were as follows: type 2 diabetes 11.1%, hypercholesterolemia (cholesterol>240 mg/dl or using cholesterol-lowering medication) 23.8%, hypertension 27.2%, current smoking 38.9% and physical inactivity 43%. Of the participants, only 21% were free of any of these factors. Clustering of two to five risk factors was more frequent among persons aged 50 years and older as compared with younger ones (60% vs 27%, P=0.000). The age-adjusted prevalence of CHD was 6.3% (in men, 8.9%; in women, 3.8%) and that of myocardial infarction was 3.6% (in men, 5.2%; in women, 2.1%). According to multivariate analysis age, gender, education level, obesity, diabetes, hypercholesterolemia, hypertension and ever smoking were strongly associated with CHD.
Conclusion:
Classic risk factors are highly prevalent and frequently clustered, especially in adults aged 50 years and older. These findings raise concerns about future trends of already increased rates of CHD. Multifactorial and integrated population-based interventions need to be applied to reduce the burden of cardiovascular conditions.
INTRODUCTION
Cardiovascular diseases (CVDs) account for the greatest burden of morbidity and mortality worldwide in both developed and developing countries. According to the latest available data from the World Health Organization, the leading causes of noncommunicable diseases deaths in 2012 were CVD (17.5 million), cancers (8.2 million), respiratory diseases (4.0 million) and diabetes (1.5 million) [1]. Moreover, there is growing awareness and concern about growing burden of CVD not just from the public health perspective but also from the economic one. In 2010, the global direct and indirect cost of CVD was approximately US$ 863 billion and is estimated to rise 22% to US$ 1,044 billion by 2030, indicating that the burden of CVD will have huge impact on health systems and the economy [2].
Coronary heart disease (CHD) is the greatest contributor to CVD and risk factors such as cigarette smoking, elevated cholesterol levels, high blood glucose, high blood pressure, physical inactivity and obesity are the driving forces behind the disease burden. Over 90% of CHD events occur in individuals with at least 1 risk factor [3, 4]. Incidence and prevalence of CHD vary greatly according to sex, geographical region and ethnic background. Comprehensive data regarding prevalence of CHD and associated factors in different geographical regions are very important to our understanding of global distribution and evolution of CHD. Moreover, implementing effective disease prevention and control strategies requires surveillance that tracks the burden of disease in the population. Few data on temporal trends of CHD and major cardiovascular disease risk factors are available from different populations [5, 6]. For Greece, the population-based data regarding CHD and associated risk factors are limited and not so comparable with each other [7-9], a phenomenon that characterizes most European countries [10].
The Seven Countries Study showed that Greece, in the 1960s, was known for having low rates of CHD morbidity and mortality as compared with northern European countries and the United States (US) [11]. In the following decades, however, the transition from the traditional Mediterranean diet and high habitual physical activity to a Western-type diet, a more sedentary lifestyle, and high smoking rates brought Greece in a position where it is no more a low-CVD risk country [7, 9]. Over the last years, Greece has been experiencing a socio-economic crisis and the evaluation of CVDs burden is of great interest from many perspectives. Thus, we sought to examine the current prevalence of CHD in combination with the prevalence of classic risk factors in a sample of adult population.
MATERIALS AND METHODOLOGY
Study Design and Data Collection
This cross-sectional survey was performed in the municipality of Saronikos, which is part of Attica region (greater Athens area). The survey took place during the election day of May 2014. The target population comprised of about 23000 adult residents of municipality of Saronikos. The same methodology has been used in previous surveys and described in relevant publications [7, 12, 13]. In particular, a team of trained interviewers (13 medical professions) performed face-to-face interviews, using an anonymous questionnaire. All voting centers in the municipality (n=6) were included in the sampling procedure, and eligible participants were selected at random. The response rate was 84%. Participants were unaware of the content of the questionnaire and there were no differences in the distribution either by gender, or by age group in the non-respondents; thus, the findings were less likely to be effected by participation bias.
The following information was initially collected: year of birth, sex, educational level and the smoking status. Current smokers were defined as persons who smoke at least 1 cigarette daily. Former smokers were defined as those who had quit smoking at least one year before the interview. The rest of the participants were defined as nonsmokers.
Participants were then asked to report if they have been diagnosed with diabetes, presence of which was confirmed by questions regarding the type of diabetes, year (or age) at diagnosis, and current mode of treatment. Additionally, respondents were asked to report their height and weight, and were thus classified as overweight if their body mass index (BMI) was between 25.0 and 29.9 kg/m² and as obese if it was ≥ 30 kg/m².
Data were collected regarding hypercholesterolemia. Participants were asked to identify the status of their total cholesterol level: <200 mg/dl, 200-240 mg/dl, >240 mg/dl or unknown. Respondents were defined as having hypercholesterolemia if they reported total cholesterol levels greater than 240 mg/dl or if they currently used cholesterol-lowering medication [14]. They were also asked if they had hypertension, and the use of medication was recorded. All participants were asked if they had a medical diagnosis of CHD [15]. Moreover, the history of myocardial infarction (MI) (including the year of its occurrence), the history of coronary bypass surgery and percutaneous coronary intervention were recorded.
In addition, participants were asked to report the number of days per week that they had participated in any form of leisure-time physical activity during the last month. The questions included the frequency of weekly moderate-intensity activities (such as brisk walking, dancing, bicycling or gardening) and vigorous-intensity activities (such as running, aerobics, swimming or heavy yard work) [16]. Respondents who reported no participation in moderate- or vigorous-intensity physical activity were classified as being physically inactive. Finally, they were asked if they had checked their blood glucose and cholesterol levels in the past years. The study was approved by the local Ethics and Scientific Committee.
Study Population
After excluding respondents aged younger than 20 years (n=47), the total number of study participants in the survey was 2636 (1306 men and 1330 women); the mean age of participants was 50.5±17.8 (range 20-95) years. There were only minor differences in the age and gender distributions between the survey and the target population (Table 1). Probably, the high voter turnout (about 73%) contributed considerably to obtain a representative sample.
Age and gender stratification of Saronikos Municipality residents who participated in the survey.
| Men | Women | Overall | |||||||
| Age (yrs) | Population* | Sample | Sampling fraction | Population* | Sample | Sampling fraction | Population* | Sample | Sampling fraction |
| 20-29 | 1531 | 210 | 0.137 | 1519 | 199 | 0.131 | 3050 | 409 | 0.134 |
| 30-39 | 2178 | 212 | 0.097 | 2249 | 219 | 0.097 | 4427 | 431 | 0.097 |
| 40-49 | 2208 | 205 | 0.093 | 2146 | 218 | 0.102 | 4354 | 423 | 0.097 |
| 50-59 | 1817 | 218 | 0.120 | 2035 | 229 | 0.112 | 3852 | 447 | 0.116 |
| 60-69 | 1765 | 206 | 0.117 | 1811 | 255 | 0.140 | 3576 | 461 | 0.129 |
| ≥70 | 1816 | 255 | 0.140 | 1899 | 210 | 0.111 | 3715 | 465 | 0.125 |
| Total | 11315 | 1306 | 0.115 | 11659 | 1330 | 0.114 | 22974 | 2636 | 0.115 |
Statistical Analyses
Data analyses were performed using SPSS 20.0. Continuous variables were expressed as mean ± SD and categorical variables were reported as percentages. Bivariate associations were assessed by Pearson chi-square test or t-test. We used the binary logistic regression to examine the crude and adjusted Odds Ratios (OR) of the association of CHD with the variables of interest. The applied model included history of CHD (yes/no) as the dependent variable, and age, gender, educational level, obesity, diabetes, hypertension, hypercholesterolemia, smoking, and physical inactivity as covariates. Statistical significance for all analyses was assessed at the level of P<0.05.
RESULTS
Prevalence of cardiovascular risk factors
Table 2 presents the levels of 5 major risk factors by age in women and men, respectively. The crude prevalence of known type 2 and type 1 diabetes was 11.9% (n=313) and 0.1% (n=2), respectively. As shown in Table 2, the prevalence of type 2 diabetes was higher in men than women (13.2% vs 10.5%, P=0.031) and increased significantly with age (P = 0.000). The mean age of diabetic patients and the mean duration of diabetes were 66.6±11 and 9.7±7 years, respectively. Eleven percent of diabetic patients reported that they were on diet alone, 67% were receiving oral antidiabetic agents alone and 22% were using injectable agents (16% insulin). The majority of participants (93%) reported that they had checked their blood glucose and cholesterol levels during the last 3 years.
The prevalence of self-reported hypercholesterolemia was 26.2% (n=640/2447), with similar rates in both sexes (27% vs 25.3%, P=0.336); the differences were significant only in subjects under 50 years of age (8.7% in men vs 3.8% in women, P=0.001). Among subjects with hypercholesterolemia, the percentage of those who were under cholesterol-lowering medication was 91% (n=582/640).
In total,758 individuals reported to be diagnosed with hypertension (28.8%) (29.2% in men and 28.3% in women, P=0.579). As shown in Table 2, the prevalence rates of hypertension are increasing with age (P=0.000). The percentage of subjects taking antihypertensive medications was 92.5% (701/758).
The percentage of current smokers was 38.9% (39.2% in men and 38.6% in women, P=0.739). The higher prevalence (52.5%) was observed in people aged 40-49 years and the lower prevalence (13.3%) was observed in 70+ years old individuals. The percentage of former smokers was 21% (26.8% in men and 15.3% in women, P=0.000).
Age- and gender-specific prevalences of major cardiovascular risk factors, the Saronikos study.
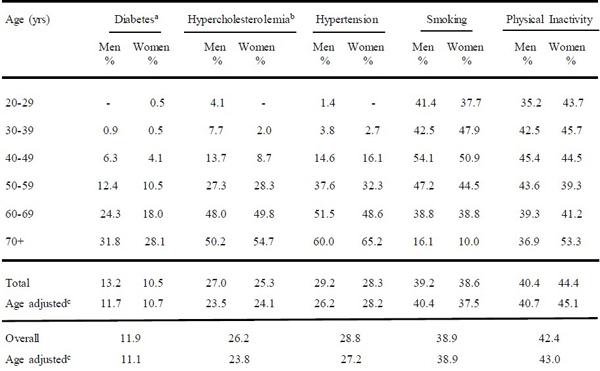 |
The percentage of adults who reported no participation in any leisure-time physical activity was 42.4% (40.4% in men and 44.4% in women, P=0.034). The differences between two sexes across age groups were not statistically significant, except in individuals 70+ years old (36.9% in men vs 53.3% in women, P=0.000). Thirty-five per cent of the participants reported that they were engaged at least three times per week in any form of leisure-time physical activity; only the proportion of 14.4% has been engaged in vigorous-intensity physical activity.
The prevalence of obesity was 21.6% and that of overweight was 42.5%. The respective percentages in men and women were: 23.5%, 50.2% and 19.8%, 34.9% (P=0.000). The percentage of obesity was almost doubled in people aged 50 years and older (28% vs 14.6%, P=0.000). The age-adjusted prevalence of obesity was 21.1% (22.8% in men and 19.6% in women).
Among 2636 adults, only 21% were free of any modifiable major risk factors, 34% had one factor, 27% had two and 18% had three to five risk factors. As shown in Fig. (1), the prevalence rates of risk factors clustering were significantly higher in people aged 50 years and older as compared with younger adults (P=0.000).
Prevalence and Associated Factors of CHD
In total, 106 individuals (4%) (5.9% in men and 2.2% in women, P=0.000) reported that they had suffered a MI; the respective age-adjusted prevalence rates were 3.6% (5.2% and 2.1%). The mean age of subjects with history of MI and the mean age of first episode was 68.8 ± 10 years and 57.3 ± 11 years, respectively. As shown in Fig. (2), the prevalence rates of MI are very low in younger adults and increased markedly after the age of 50.
The prevalence of diagnosed CHD was 7.1% (10.3% in men and 3.8% in women, P=0.000); the respective age-adjusted prevalence rate was 6.3% (8.9% in men and 3.8% in women). Of 186 individuals with recognized CHD, 58 (31%) and 63 (34%) reported that had undergone coronary bypass surgery and percutaneous coronary intervention, respectively. The mean age of patients with CHD was 70.1 ± 10 years.

Prevalence of clustering of major cardiovascular risk factors in the age groups of <50 and ≥ 50 years, the Saronikos study.
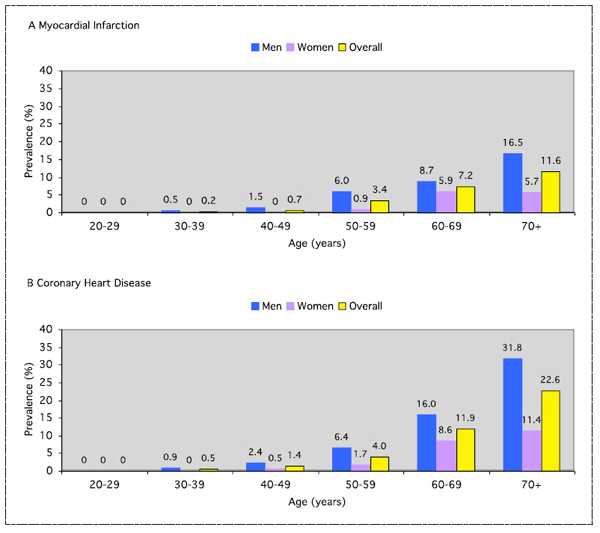
Age- and gender-specific prevalence of MI and CHD among Greek adults aged 20 years and older, the Saronikos study.
As shown in Table 3, all studied risk factors, except inactivity, were significantly associated with the presence of CHD. The separate multivariate analysis for men and women revealed that there were no gender differences in the magnitude of relationship between risk factors and established CHD.
Prevalence rates of self-reported CHD and effects of potential risk factors in a sample of Greek adults, the Saronikos study.
| % | Crude OR ( 95% CI) | P | Adjusted OR (95% CI) | P | |
| Age (per year) | 1.09 (1.08-1.11) | 0.000 | 1.08 (1.06-1.10) | 0.000 | |
| Gender | |||||
| Women † | 3.8** | 1.00 | 1.00 | ||
| Men | 10.3 | 2.89 (2.07-4.03) | 0.000 | 2.65 (1.79-3.92) | 0.000 |
| Educational level | |||||
| Higher † | 4.2** | 1.00 | 1.00 | ||
| Moderate | 6.4 | 1.58 (1.06-2.33) | 0.024 | 1.30 (0.85-1.97) | 0.227 |
| Low | 13.8 | 3.69 (2.53-5.38) | 0.000 | 1.62 (1.07-2.43) | 0.022 |
| BMI (kg/m2) | |||||
| <25 † | 3.2** | 1.00 | 1.00 | ||
| 25-29.9 | 8.8 | 2.96 (1.95-4.50) | 0.000 | 1.49 (0.95-2.33) | 0.082 |
| ≥30. | 10.0 | 3.39 (2.15-5.35) | 0.000 | 1.66 (1.02-2.70) | 0.041 |
| Diabetes | |||||
| No † | 4.9** | 1.00 | 1.00 | ||
| Yes | 23.3 | 5.95 (4.31-8.22) | 0.000 | 2.88 (2.05-4.06) | 0.000 |
| Hypertension | |||||
| No † | 3.2** | 1.00 | 1.00 | ||
| Yes | 16.5 | 5.88 (4.27-8.09) | 0.000 | 1.93 (1.35-2.75) | 0.000 |
| Hypercholesterolemia | |||||
| No † | 2.2** | 1.00 | 1.00 | ||
| Yes | 22.7 | 13.3 (9.20-19.2) | 0.000 | 5.50 (3.68-8.23) | 0.000 |
| Smoking habit | |||||
| Non smokers † | 4.0** | 1.00 | 1.00 | ||
| Ever smokers | 9.1 | 2.42 (1.70-3.45) | 0.000 | 2.43 (1.61-3.29) | 0.000 |
| Inactivity | |||||
| No † | 7.4* | 1.00 | 1.00 | ||
| Yes | 6.6 | 0.89 (0.66-1.21) | 0.452 | 0.82 (0.59-1.14) | 0.241 |
DISCUSSION
The estimation of CVD burden is a dynamic research field and it is difficult to obtain a comprehensive picture. The present study provides an important update on the level and distribution of cardiovascular risk factors by age and sex in the Greek population. We observed that 8 out of 10 adults have at least one major modifiable risk factor for CVD.
In particular, the age-adjusted prevalence of type 2 diabetes was high (11.1%), indicating that it has been raised steadily during the last decade (from 8.2% in 2002 to 9.5% in 2006) [13]. In line with these findings, Andrikopoulos et al. [17] found the prevalence of known diabetes to be 9.8% (in 2004-11). According to the Attica study [18], there was an escalating increase of diabetes incidence over the period between 2002 and 2012, which was mainly a result of obesity, population aging and genetic predisposition (family history of diabetes). In comparison with other Mediterranean countries, the prevalence of known diabetes in Greece is among the highest reported: 5.5% in France (2012) [19], 8.5% in Lebanon (2008-9) [20] and 9% (16.5% of both known and unknown diabetes) in Turkey (2010) [21]. The finding that the vast majority (96%) of adults older than 45 years have recently checked their blood glucose level indicates that the diabetes awareness is high and the proportion of unknown diabetes probably is relatively low in Greek population; this is an additional reason that should be taken into account when comparing data from other countries.
Our study shows that hypercholesterolemia affects about 24% of Greek adults, indicating a rising tendency in comparison with the previous data (21% in 2006) [7]. Of note, the proportion of adults taking statins had tripled over the past 12 years (from 7% in 2002 [7], to 13% in 2006 [7] and 22% in 2014), which probably reflects the increased adherence to guidelines and the better management of hypercholesterolemia over time. A similar figure to ours was observed in the US where self-reported use of cholesterol-lowering medications increased from 8.2% in 1999-2000 to 14% in 2005-6 [22] and reached 23% in 2007-10 [23].
The age-adjusted prevalence of hypertension was 27.2%, without significant differences between men (26.2%) and women (28.2%) (Table 2). In comparison with the past years there is an upward trend (from 19% in 2002 [7] to intermediate prevalence of 24% in 2006 [7] and 25% in 2004-11 [17]). However, the percentage of individuals with diagnosed hypertension who reported taking blood pressure-lowering drugs appears to have remained roughly stable over the last decade (92% in 2006 [7] and 92.5% in 2014).
Smoking prevalence in Greece is among the highest in the world and constitutes one of the most alarming public health issues [24]. Our study shows that the prevalence of current smoking in the overall population remains too high and has declined slightly from 40.1% in 2006 [7] to 38.9% in 2014. Meanwhile, our data show a clear decreasing trend in men (from 49% in 2006 to 40% in 2014) and increasing trend in women (from 31% in 2006 to 37.5% in 2014). These results are in agreement with the study of Filippidis et al. [24], who found that no significant change in the overall prevalence of smoking was documented between 2006 and 2010 (from 43.1% to 42.6%); however, they found a decrease in the proportion of Greek men who smoke (from 52.4% to 45.4%) and an increase among women (from 34.5% to 39.8%). During the past five years, a series of legislative measures and initiatives have been implemented in an effort to reduce tobacco consumption in Greek population. Although these policies have contributed to the reduction of per capita cigarette consumption and to the increase of the intention to quit [24, 25], the above-mentioned data indicate that they did not have the anticipated results on declining of overall smoking prevalence. Probably the psychosocial consequences of financial crisis do not favor the efficient implementation of anti-smoking strategies [25, 26]. Lowering smoking rates, therefore, should remain a priority in Greece and further efforts to enforce the anti-smoking programs [27] and effective measures such as taxation and smoking banning [28] would be needed.
The available evidence showed that prevalence of physical activity and exercise in Greece during 1990s and 2000s was one of the lowest in the European Union (EU) [29]. The results of the current study show that a high proportion of adults (43%) are physically inactive, indicating that sedentary lifestyle is a major health problem for Greece. According to our data, the prevalence of inactivity declined from 56.5% in 2006 [7], while the proportion of those engaged in any form of physical activity for at least three times per week was increased from 18% in 2006 to 35% in 2014. Also, other studies are showing a similar decline in prevalence of inactivity over the last 12 years (from 58% in 2001-2 [30] to 42% in 2004-11 [17]). Meanwhile, it is essential to keep in mind that physical activity varies with season [31] when comparing results from different studies. Importantly, there was no increase in self-estimated obesity during the period from 2006 (21%) [7] to 2014 (21%). Similar results were observed in another study from Greece [32], indicating that the prevalence might have been stabilized.
The results of the present study show that the high burden of cardiovascular risk factors is accompanied by a high prevalence of CHD in adults older than 50 years of age (Fig. 2). We found that overall age-adjusted prevalence of CHD and MI was 6.3% and 3.6%, respectively. Similar prevalence rates were found among US adults (CHD, 6.2% in 2009-12; MI, 4.0% in 2013) [5]. According to comparable data from Germany (2008-11), the prevalence of self-reported CHD was 9.3% and MI 4.7% among persons aged 40-79 years [10]; in our study these rates among Greek counterparts were 9.1% and 5.3%, respectively.
Early epidemiologic data showed that in 1960s Greece had one of the lowest prevalence of CHD worldwide [11]. After 1970s, the unfavorable changes in risk factors caused a marked increase of CVD morbidity and mortality [7, 9, 33, 34]. The moderate to high levels of major risk factors such as glucose ≥120 mg/dl (6%), cholesterol ≥ 260 mg/dl (24%), blood pressure ≥140/90 mmHg (28%) and smoking >3 cigarettes/day (39%) have been observed in urban adult population since early 1980s [33, 35]. However, according to Moulopoulos et al. [33], the proportion of individuals with a certain diagnosis of CHD was very low (1.6%) and the prevalence of MI was 1.1%; meanwhile, it should be noted that the authors of the study found an additional proportion of cases (1.9%) with a doubtful diagnosis of CHD. Comparing these rates with those of our study, there was a 3.9-fold increase in CHD and 3.3-fold increase in MI from 1980 to 2014. These observations are in line with the findings of the Attica study, which suggests a progressive increasing trend in incidence of CVD during the last decades [9]. In addition, national trends on hospitalization rates for all forms of CHD [36] reinforce the above observations. As shown in Fig. (3), the number of hospital discharges was steadily increased for about three decades: from 28556 in 1980, reaching to the highest peak of 108165 in 2006 (3.8-fold increase), and subsequently declined to 94316 in 2010 (3.3-fold increase). Undoubtedly, the rising burden of CHD is mainly driven by the prolonged exposure to high levels of CVD risk factors; however, the population aging and the increasing of diagnosis of CHD as result of widespread use of more sensitive diagnostic techniques should be considered when comparing current prevalence rates with those of the early 1980s. The reasons for decline in hospital discharges between 2006 and 2010 are not clear. However, based on so far available data [7, 9, 17, 18], which are showing no significant reduction in prevalence and incidence of main CVD risk factors, we speculate that this decline is mainly due to better detection and increased use of medical treatments such as pharmacotherapy and coronary revascularization. The experience of other developed countries suggests that this decrease in CHD hospitalization rates could have been even greater, if the increased use of cardio-protective medication was associated with higher smoking reduction and promotion of healthy lifestyles [37]. Taking into account the growing levels of risk factors and especially the frequent clustering of them (Fig. 1), it is obvious that a sizeable proportion of Greek population has a high risk for future coronary events. Considering the healthcare costs, this imposes a significant burden on already stressed healthcare system and Greek economy, and it may become even more serious unless a comprehensive, coordinated approach is taken [38].
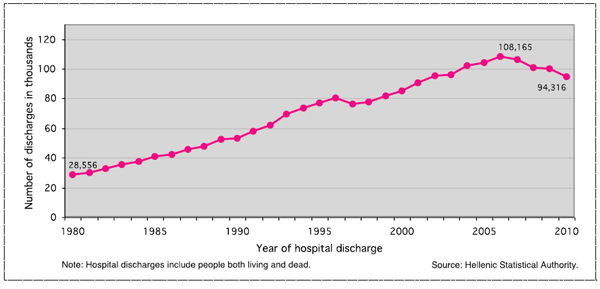
Trends in hospital discharges for CHD in Greece, 1980 – 2010
Sufficient evidence indicates that the prevalence and incidence of CHD have declined or at least stabilized in the Western world, and this is thought to be attributable to reductions in major risk factors including smoking, cholesterol and blood pressure [10, 39-41]. Also, deaths from CHD have been decreasing in most developed countries over the last decades [41-43]. In the Seven Countries Study, the 40-year CHD mortality tended to decline in the US, Finnish, Dutch and Japanese cohorts and exponentially increased in cohorts of Serbia and Greece [43]. The acceleration in mortality risk in the latter countries corresponded to the largest score of risk factors change. On the contrary, the Northern European countries showed opposite trends in behavior and lifestyle. It is largely documented that these countries have succeeded in reducing the risk factor levels of the population and declining the incidence rates of CHD due to energetic and comprehensive prevention policies over many decades, including promotion of smoking cessation and more healthy diets [39, 40, 42-44].
Our study confirms that age, gender, education level, obesity, diabetes, hypercholesterolemia, hypertension and ever smoking are strongly and consistently associated with CHD [3, 4, 45]. The modifiable factor that showed the greatest magnitude of association with CHD was hypercholesterolemia (adjusted OR: 5.50) followed by type 2 diabetes (adjusted OR: 2.88), ever smoking (adjusted OR: 2.43), hypertension (adjusted OR: 1.93) and obesity (adjusted OR: 1.66). Of note, the individuals with diagnosed CHD have significant lower prevalence of current smoking in comparison with the rest of the population (24% vs 40%) and the highest rate of former smokers (55% vs 18%, P=0.000), confirming that diagnosis of CHD is a powerful stimulus for smoking cessation [46, 47]. A similar pattern seems to occur with regard to the leisure-time physical activity, as many patients with CHD tend to abandon the sedentary behavior and adopt a more physically active lifestyle after a cardiac event [48]. Probably, this phenomenon explains the finding of the present study that the prevalence of physical inactivity does not differ significantly between the patients with CHD and the general population (40% vs 43%, adjusted OR=0.82, P=0.241).
These data underscore the importance of modifiable risk factors in the prevention and development of CHD. From the INTERHEART study that included 52 countries, it is estimated that modifiable risk factors account for about 90% of the population-attributable risk for heart disease [45]. Furthermore, numerous intervention studies suggest that an enormous amount of CVDs can be prevented by adopting healthy behaviors or by optimizing behavioral and clinical risk factors [49-52]. Thus, a greater focus on lifestyle modifications such as quitting smoking, losing weight, eating a healthy diet and taking exercise must be the cornerstone of the public health strategies for reducing the growing burden of CVD risk factors in the Greek population. Creating more walkable places and other actions related to the urban environment that aim on promoting active living is essential component of a national plan for successful implementation of those strategies [53]. In addition, regulations at national and EU level for restrictions of marketing foods and drinks that are high in sugar, salt and trans fats will also contribute in the prevention of obesity, diabetes, hypertension, dyslipidemia and CHD [54-56].
Our study has some limitations. Firstly, the presented data were relied on the self-reported information, which may underestimate the true prevalence of conditions of interest. However, the evidence shows that the self-reported data concerning well-known traditional risk factors are reliable. Self-reported data compared with medical records show almost perfect agreement for diabetes, and substantial agreement for hypertension and hypercholesterolemia [57-59]. Also, the validity of self-reported cardiac events including diagnosed MI, angina, percutaneous coronary intervention and coronary bypass surgery is likely to be very high [59, 60]. In regards to obesity, observational and experimental studies on adult populations have demonstrated that self-reported height and weight correlate well with measured values, although individuals tend to overestimate their height and underestimate their weight. A recent population-based study from Australia has shown that the prevalence of overweight based on self-reported data was comparable to that based on measured values, while the prevalence of obesity was underestimated by around 6% [61]. Secondly, we also acknowledge that our results are based on cross-sectional analysis, therefore, the causal effect of risks factors such as physical activity that tend to change after diagnosis of CHD could not be evident. Finally, although our population is quite representative in terms of age-, sex- and educational level - distribution of the residents living in greater Athens area, generalization of the present results to all Greek population should be made with caution. Despite the limitations, this study provides important data to inform current clinical practice, policy making and future research targeting on CVD. To our knowledge, this is the first community-based study of its kind referring to prevalence rates of CHD and associated factors in the Greek population.
CONCLUSION
The results of our study have clearly shown that among Greek adults there is a high prevalence of diabetes, hypertension, hypercholesterolemia, smoking and physical inactivity, which are all major modifiable risk factors for CHD. The study also highlights the frequent clustering of risk factors, especially in adults aged 50 years and older, suggesting that a sizeable proportion of our population has a high risk for coronary events. These findings raise concerns about future trends of already increased rates of CHD. From the perspective of public-health service, the appropriate management of such burden of cardiovascular conditions at lower cost is a big challenge. Thus, multifactorial and integrated interventions to reverse this situation, focusing on smoking cessation, promotion of traditional Mediterranean diet, and increasing physical activity, are urgently needed.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We thank all the health professionals who participated in the interviewing process as well as the local authorities’ representatives who helped in the completion of this study.


