All published articles of this journal are available on ScienceDirect.
Does Stroke Volume Increase During an Incremental Exercise? A Systematic Review
Abstract
Introduction:
Cardiac output increases during incremental-load exercise to meet metabolic skeletal muscle demand. This response requires a fast adjustment in heart rate and stroke volume. The heart rate is well known to increase linearly with exercise load; however, data for stroke volume during incremental-load exercise are unclear. Our objectives were to (a) review studies that have investigated stroke volume on incremental load exercise and (b) summarize the findings for stroke volume, primarily at maximal-exercise load.
Methods:
A comprehensive review of the Cochrane Library’s, Embase, Medline, SportDiscus, PubMed, and Web of Sci-ence databases was carried out for the years 1985 to the present. The search was performed between February and June 2014 to find studies evaluating changes in stroke volume during incremental-load exercise. Controlled and uncontrolled trials were evaluated for a quality score.
Results:
The stroke volume data in maximal-exercise load are inconsistent. There is evidence to hypothesis that stroke volume increases during maximal-exercise load, but other lines of evidence indicate that stroke volume reaches a plateau under these circumstances, or even decreases.
Conclusion:
The stroke volume are unclear, include contradictory evidence. Additional studies with standardized reporting for subjects (e.g., age, gender, physical fitness, and body position), exercise test protocols, and left ventricular function are required to clarify the characteristics of stroke volume during incremental maximal-exercise load.
INTRODUCTION
The cardiac performance is based on satisfactory left ventricular (LV) function to ensure a blood output to all tissues. Thus, LV function increases to maintain homeostasis according to metabolic load [1]. During an incremental-load exercise, cardiac output should increase to meet the extraordinary blood demands of the working musculature. This additional blood flow provides the major capability for acting exercise. The manner in which the LV responds to the strain of exercise has intrigued physiologists. In fact, exercise training requires a fast adjustment in heart rate and stroke volume (SV) [1].
The heart rate is a mechanism by which cardiac output rises during effort under physiological conditions. It is well known that heart rate increases linearly with exercise load because of an imbalance between sympathetic and parasympathetic autonomic nervous activity. There are two major mechanisms by which tachycardia occurs during incremental exercise: (1) decreased parasympathetic restraint and (2) increased sympathetic drive. The SV increase is linked to two different situations: (1) low-exercise load, in which the Frank-Starling mechanism has a key role and (2) increased myocardial contractility, shown to occur under maximal-load exercise (MLE) [2, 3].
Currently, the nonlinear SV response to increases in the exercise load is an issue of interest. Studies using several experimental approaches have shown decreases, plateaus, or increases SV during MLE. In the light of these findings, this systematic review incorporates original articles that assessed changes in SV during incremental-load exercise, to exhaustion, in healthy adult humans.
MATERIALS AND METHODS
Search Procedure
A comprehensive review was carried out of the Cochrane Library’s, Embase, Medline, SportDiscus, PubMed, and Web of Science databases for studies published since 1985. The search was based on the following keywords and MeSH terms: aerobic exercise, cardiac output, dynamic exercise, incremental exercise, health subjects, hemodynamic, maximal effort, stroke volume, and systolic function. The search sentences were combined to increase the results.
The survey was carried out between February and June 2014. All studies evaluating the changes in SV during an incremental-load exercise were selected. Two independent researchers using a double-blind approach performed the analyses. The first step of the search was to analyze the abstracts in the database according to the following criteria: participant profile, trial design, exercise test procedure, and SV evaluate approch.
Inclusion and Exclusion Criteria
Controlled and uncontrolled trials published in peer-reviewed journals were included. We included only trials published in English, conducted on healthy subjects, and which included full information about the physical test procedure and approach used to measure SV. Trials containing supplemented diets, diseased subjects, reviews, and case reports were excluded because they did not express the normal baselines. Studies that did not report their experimental design or outcomes were also excluded.
Studies without clear detailing of SV approaches, as well as exercise protocol were excluded. We evaluated only studies that assessed SV up to a MLE. All eligible articles were reviewed and critically evaluated for quality scores, as previously reported in detail [4, 5].
RESULTS
the Details for screened studies are shown in Fig. (1). In the first screening, we have found 336 articles there were no differences in database search between the two researchers. The abstracts were used to examine duplication in the database. After a search filter application, 144 studies were found. Of these, 131 articles were excluded because they did not meet the eligibility criteria or quality scores.
A total of 13 articles were selected for critical data analysis, and the results are shown in Table 1. Several different incremental exercise-load protocols were used in these studies to induce a maximum effort level. In summary, ten studies measured effort level on a cycle ergometer, two with treadmill running, and one with a 100-drop-jumps protocol. Moreover, the studies used several approaches to evaluate SV. Four studies used cardiac impedance, three used acetylene rebreathing, two used radionuclide ventriculography, and three used catheterization. Only one study applied a predictive equation to evaluate SV. In respect to LV performance, we found conflicting information for SV during MLE. Several investigations found a SV plateau at a submaximal-exercise load, [6-10] followed by a 40%-50% decrease in VO2max or a decrease in heart rate of 120 bpm [6-10, 13]. These findings applied mostly to sedentary and moderately active subjects. On the other hand, athletes showed an increased SV during MLE [13-15].
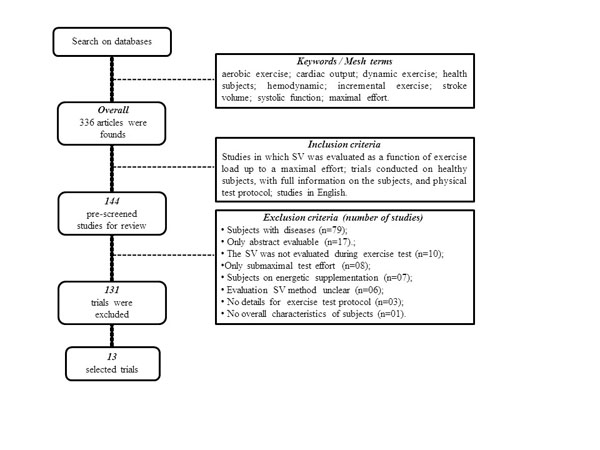
Flow diagram for search procedure and selection of manuscript included in the systematic review.
DISCUSSION
This study is the first systematic review to evaluate SV changes during incremental-load exercise. Overall, we found conflicting information regarding SV during MLE. The available evidence shows an increase, as well as a plateau or a decrease, in SV.
Gledhill et al. [15] support the hypothesis that trained subjects show an increased SV during MLE, whereas untrained subjects show a plateau at an early phase of exercise with the same exercise load. Several lines of evidence indicate SV increases to between 91% and 100% of VO2max in endurance athletes [16-22]. In contrast, there are doubts to SV during MLE in moderately trained subjects, with an SV plateau at submaximal-exercise intensity [23]. We found only one study that showed an increase in SV in nonathletic subjects [24]. This evidence indicates that a high level of physical fitness may be required to obtain increased SV during MLE.
Several mechanisms have been related to a higher SV in athletes during MLE (Fig. 2): increased diastolic filling, LV cavity dimensions, E/A ratio and transmittal pressure gradient, improved myocardial compliance, developed pressure rate (dP/dt), and sarcoplasmic reticulum function [15, 16, 21, 25, 26].
In respect to a SV plateau (Fig. 2), two issues have been shown to be important [6-11, 15]: (1) at a low-exercise load, LV filling pressure and end-diastolic volume (Frank-Starling mechanism) increases are linked to a higher SV; (2) at a high workload, an increased heart rate is followed by a decrease in the end-diastolic volume despite an increase in filling pressure. Therefore, SV may be sustained by a decrease in the LV end-systolic volume.
Studies enrolled in the systematic review.
| Trials | Sample | Exercise Protocol | SV Approach | Result |
|---|---|---|---|---|
| Fukuda et al. (2010), Japan | 9 untrained men (30.3±8.5 yr) | Cycle ergometer | Cardiac impedance | SV increased on MLE |
| Lewis et al. (2008), USA | 8 active men (20.7±0.4 yr) | Cycle ergometer | Cardiac impedance | SV increased on MLE |
| Marcora et al. (2008), England | 10 active men (23±4 yr) | 100-drop-jumps protocol | Cardiac impedance | SV reached a plateau on SLE |
| Stickland et al. (2006), Canada | 8 active men (29.7±2 yr) | Cycle ergometer | Radial artery catheter and a Swan-Ganz catheter | Subjects with VO2max < 55ml.kg-1.min-1 showed a plateau or a decrease in the SV on SLE. Subjects with VO2max > 55 ml.kg-1.min-1 showed SV increases on MLE |
| Stringer et al. (2005), USA | 5 active men (25 style="background-color: white">±6 yr) | Cycle ergometer | Cardiac catheterization by flow-directed balloon catheter | SV reached a plateau on SLE; SV decreased on MLE |
| Dufour et al. (2004), France | 8 active men (28±2 yr) | Cycle ergometer | Cardiac impedance | SV reached a plateau on SLE |
| Warburton et al. (2002), Canada | 10 trained men cyclists | Cycle ergonometer | Radionuclide ventriculography | SV increased on MLE |
| Zhou et al. (2001), USA | 5 elite runner men (29.8±5.2 yr); 10 university runner men (25.5±4.3 yr); 10 untrained men (28.1±7.5 yr) | Treadmill running | Acetylene rebreathing | Untrained and moderately active subjects: SV reached plateau on SLE. Elite athletes: SV increased on MLE |
| McCole et al. (1999), USA | 24 women: 8 sedentary, 10 active, and 6 master athletes (63±5 yr) | Treadmill running | Acetylene rebreathing | SV decreased on SLE |
| Stringer et al. (1997), USA | 5 active men (25±6 yr) | Cycle ergometer | EQUAL: SV was estimated if the C(a-vDO2); | SV reached a plateau on submaximal exercise load; SV decreased on MLE |
| Gledhill et al. (1994), Canada | 7 trained men (22.5±2.1 yr) and 7 untrained men (22.2±4.9 yr) | Cycle ergometer | Acetylene rebreathing | Untrained: SV reached a plateau with 120 bpm. Trained: SV increased until the HRmax |
| Stratton et al. (1994), USA | 17 young (28±3 yr) and 15 active old men (68±6 yr) | Cycle ergometer | Radionuclide ventriculography | SV reached a plateau on SLE; SV decreased on MLE |
| Higginbotham et al. (1986), USA | 24 men: 9 active and 15 sedentary (20-50 yr) | Cycle ergometer | Cardiac catheterization by 7-French balloon-tipped thermodilution Swan-Ganz catheter | SV reached a plateau on SLE |
bpm, beats per minute; HRmax, maximal heart rate; MLE, maximal load exercise; SLE, submaximal load exercise; SV, stroke volume; VO2max, maximal oxygen consumption.
Authors whose results support a lower SV during MLE report that the decline coincides with a plateau or decrease in cardiac output, resulting from the regulatory limitations of the heart (Fig. 2) [12]. This decrease is linearly related to increases in core temperature, catecholamines, heart rate, and blood pressure. Hence, SV declines could be a result of several factors linked to a preload depression of and/or decrease in LV ejection [27]. Moreover, one line of evidence supports the hypothesis that SV reduction during MLE could be related to the restrictions on LV filling time and LV end-diastolic volume that accompany tachycardia [28]. Cardiovascular strain associated with dehydration and hyperthermia may also decrease SV [29, 30].
In summary, studies have shown increases, plateaus, and decreases in SV during exercise at submaximal to maximal workloads. These findings are clearly inconsistent and must be resolved by future investigations. Our analysis can help to explain the divergent results. A detailed article analysis revealed the several exercise protocols were applied to induce high SV levels. Moreover, several approches (e.g. invasive/noinavsive) were used to evaluate SV. A more detailed analysis of the results in Table 1 shows that the available data were obtained from subjects differing in age, gender, physical fitness level, and body position during the experiments. As LV function is known to be affected significantly by these factors [21, 31, 32], it remains unclear how SV changes during MLE.
LIMITATIONS OF CURRENT KNOWLEDGE
As a systematic review, our study cannot disregard the design and/or execution problems linked to selected primary studies. Moreover, it is possible that the lack of study homogeneity may have influenced the interpretation of the results. Thus, limitations relating to the heterogeneity of approaches to SV analysis should also be exposed; some results may be inconclusive when several studies are compared to each other. These issues show to be considered for the current knowledge on the SV performance during exercise at submaximal to maximal loads. Ultimately, we only included studies published in English, which may have excluded relevant studies in other languages.
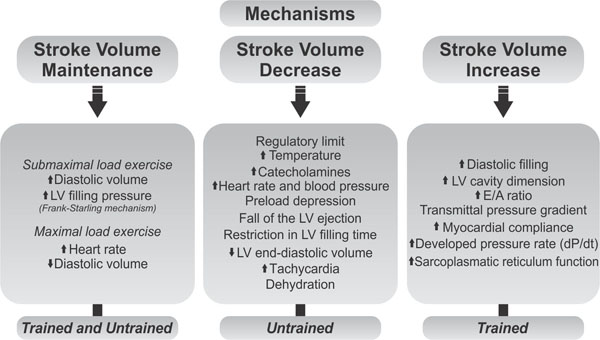
Regulatory stroke volume mechanisms under low/moderate and high exercise loads.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
This work was partially supported by grant number 479395/2012-8, National Council for Scientific. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors are grateful to American Manuscript Editors for professionally editing this paper.


